

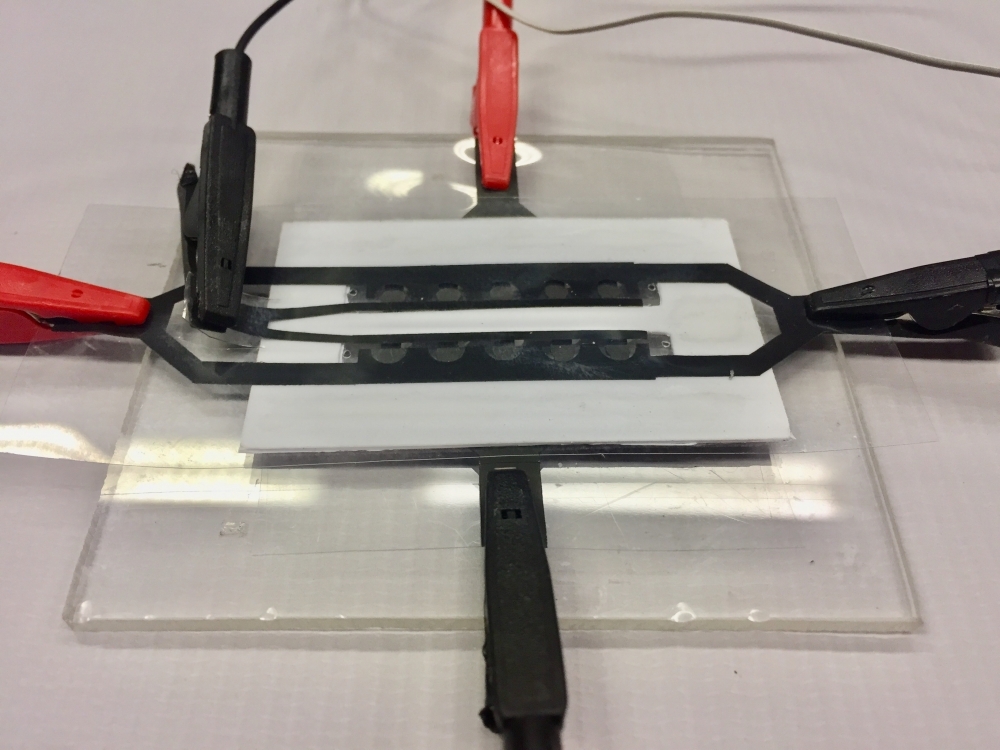
The device will identify parts of the virus’s RNA in the saliva of infected subjects. Other initiatives by the research group at the Federal University of São Carlos include developing sensors to look for the pathogen in the air and in sewerage systems (photo: UFSCar)
Published on 03/23/2021
By Maria Fernanda Ziegler | Agência FAPESP – Researchers at the Federal University of São Carlos (UFSCar) in the state of São Paulo, Brazil, are developing devices to detect the novel coronavirus SARS-CoV-2 in infected patients, contaminated environments, and even sewers.
The project calls for the use of an electrochemical sensor capable of detecting at least three viral RNA sequences in saliva samples. It is supported by FAPESP under the call for proposals entitled “Fast-track supplements for projects against COVID-19”.
“Our goal is to develop a simple low-cost method of diagnosing COVID-19. The test will be disposable, and will use easily acquired materials and simple equipment. It will also be capable of analyzing several samples simultaneously,” said Ronaldo Censi Faria, a researcher in UFSCar’s Center for Exact Sciences and Technology, and principal investigator for the project.
According to Faria, the rapid test device will have several compartments (technically called microfluidic channels) for insertion of saliva samples. Each compartment will have four independent sensing regions with chips programmed to identify viral RNA sequences.
“The virus is detected by electrogenerated chemiluminescence, or ECL, where light is emitted by the sensor’s electrochemical reaction with viral RNA. If the sensor detects at least one RNA sequence, a light appears to show that the subject is infected,” he said.
In 2017, Faria and his group developed a similar device to detect biomarkers of Alzheimer’s disease. “We normally work with physicians and specialists in other areas who present a problem to us. In the case of the Alzheimer’s device, Márcia Cominetti, a professor in UFSCar’s Gerontology Department, contacted us after observing that a protein present in the blood [ADAM10] was altered in patients with Alzheimer’s,” Faria recalled.
In response to this information, the group developed a sensor to detect the protein. The device is inexpensive and has been patented, but there are no plans to market it yet.
Protein biomarkers
The methodology used to develop COVID-19 tests is an adaptation of a series of devices that are being developed in laboratories to detect cancer, leishmaniasis, leprosy, Zika and Alzheimer’s, Faria explained.
“Our lab has experience with the use of protein biomarkers for disease detection,” he said. “Some were already well known, others were novel, as in the case of our Alzheimer’s device. In this new project, we’ll use RNA markers, parts of the RNA sequence that have been separated by Matias Melendez, a researcher who belongs to our group.”
In the study of COVID-19, the researchers will initially test the application of genetic biomarkers in samples with synthetic sequences. In phase two of the project, the technique will be validated in samples from patients diagnosed with the disease by UFSCar’s teaching hospital, via a collaboration between Faria and Henrique Pott Junior, a professor in the Department of Medicine.
Identifying the virus in environments
The multidisciplinary team is also developing other tests involving sensors to detect the virus in environments such as homes, streets and offices, as well as in sewers. These two other projects are supported via a call for proposals by Brazil’s National Council for Scientific and Technological Development (CNPq).
“We already have a methodology, so it’s in our interest to adapt it to different uses, provided a biomarker can be identified for a disease,” Faria said.
In addition to its work on the detection of viral RNA sequences, the group is also pursuing a different approach that centers on the capsid, the protein shell that encases the viral genome. “If we can detect the capsid, we can develop a more comprehensive test requiring less sample treatment,” he explained.
A solution is needed to “break open” the virus and expose its RNA for detection by the sensor, Faria added. “When the capsid is identified, it will be possible to detect the virus directly, opening up an array of possibilities such as creating a device to detect it in sewers or in the air,” he said. “This could be used to monitor the external environment remotely and map contamination of areas by sewage or particulate matter in the atmosphere.”
Source: https://agencia.fapesp.br/33298