

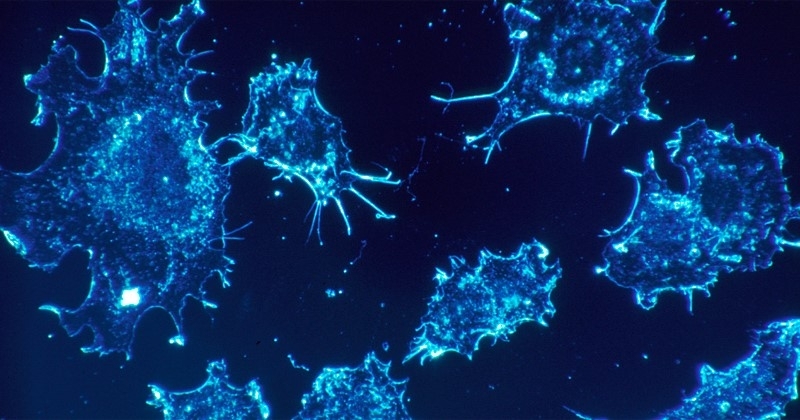
Research that can increase Brazil’s access to CAR T-cell therapy, an increasingly important strategy for treating cancer, is under way at the University of São Paulo’s Center for Cell-Based Therapy (CTC) in Ribeirão Preto, and the Butantan Institute (image: NCI-NIH/Wikimedia Commons)
Published on 07/04/2022
By Theo Ruprecht | Agência FAPESP – Defense cells are removed from the patient, genetically reprogrammed in the laboratory and re-infused to combat cancer. This is chimeric antigen receptor (CAR) T-cell therapy. The strategy is as complex as it is promising. The good news is that the Center for Cell-Based Therapy (CTC), hosted by the University of São Paulo in Ribeirão Preto (Brazil), has achieved progress with more affordable treatment of this type and is investigating similar cell-based therapies.
“Since 2019, we’ve treated seven patients, all as compassionate cases, with CAR T-cell therapy developed at our center. The results have been positive, and we plan to do more research with a view to offering more affordable treatment nationwide,” said Rodrigo Calado, one of CTC’s principal investigators and Scientific Director of the Ribeirão Preto Blood Center.
Brazil’s first CAR T-cell therapy for acute lymphoblastic leukemia and diffuse large B-cell lymphoma was produced by Novartis and approved in February by ANVISA, the national health surveillance agency. Treatment of the same kind developed by Janssen-Cilag for multiple myeloma was approved in April. In the United States these therapies cost around USD 400,000. The cost in Brazil has not yet been determined.
“We expect to be able to offer an alternative that costs between 10% and 15% of the current market price,” Calado said.
Significant savings would come, among other factors, from the ability to perform the entire process in Brazil using proprietary technology. The therapy requires collection of the patient’s own T-cells and genetically modifying them to express molecules capable of identifying the cancer cells. These CAR T-cells are then expanded (multiplied) and infused into the patient. The expected result is a more aggressive response to the cancer (more at: agencia.fapesp.br/31675).
Genetic manipulation of T-cells requires appropriate infrastructure and advanced knowledge. Moreover, the Novartis therapy approved in Brazil entails deep-freezing of the cells for transportation to the United States, where they are processed before returning to Brazil. Shipping and processing costs are therefore high.
CTC is currently preparing for publication an article on the first compassionate cases treated at the institution. “The most important message of this undertaking is that we’ve succeeded in developing a Brazilian technology to offer CAR T-cell therapy,” said Renato Cunha, a researcher at CTC and head of the Bone Marrow Transplant and Cell-Based Therapy Service at the general hospital (Hospital das Clínicas) run by the Ribeirão Preto Medical School (FMRP-USP). The treatment is currently being validated with ANVISA. “As soon as we have their go-ahead, we’ll begin clinical trials to obtain the necessary registrations,” Cunha said.
Clinical trials require a rigorous methodology, a large number of volunteers and complex infrastructure. In this case, funding has been provided by FAPESP under the aegis of its Science for Development Program.
Infrastructure
One of the centers approved in the first Science for Development call is the Nucleus for Cell Therapy (NuTeC). “Physically speaking, it consists of two buildings, one in São Paulo and the other in Ribeirão Preto,” Calado said.
The São Paulo building was opened in June 14 by Governor Rodrigo Garcia. The Ribeirão Preto building, which hosts the Nucleus for Advanced Therapy (Nutera), was unveiled on June 20, also by Gov. Garcia.
Staffed by researchers from FMRP-USP and Butantan Institute, the center plans to scale up production of CAR T-cells and other cell-based therapy products, provide support for pre-clinical and clinical trials, and develop innovative immunotherapies.
This infrastructure will enable CTC to comply with ANVISA’s requirements for clinical trials and large-scale production if the therapy is approved in future, and to partner with other public and private institutions. “The center provides a bridge between scientific knowledge and the supply of a therapy for the general public,” Calado said. The facilities in Ribeirão Preto and São Paulo have the capacity to treat 300 patients per year.
“We want to become a hub for production of this type of cell. For some kinds of cancer, CAR T-cells can produce highly positive responses even in advanced-stage patients after all other options have failed. Guaranteeing access to this treatment is important for a country like Brazil,” Cunha said.
Advances and combinations
CAR T-cell therapies have so far been approved only for certain blood cancers, such as leukemia and B-cell lymphoma. According to a review by a German researcher, the technique achieved long-term results only in 4% of patients with solid tumors (breast, prostate, lung cancer etc). Another article points to only 1%.
“Solid tumors in general produce molecules that promote local immunosuppression by inhibiting the action of conventional defense cells and CAR T-cells,” said Lucas Botelho de Souza, head of CTC’s Gene Transfer Laboratory. These molecules are known as immune checkpoints.
The last decade has seen the development of immunotherapy drugs that inhibit these checkpoints, considerably improving the treatment of several types of cancer, even at an advanced stage. “However, sometimes the results aren’t as good as expected because the body’s natural T-cells may not recognize the disease as an enemy,” Botelho de Souza said.
In light of this problem, researchers have studied the combined use of CAR T-cells with checkpoint inhibitors. The idea is that the drugs remove the blockage put in place by the cancer, while the cells lead an intense personalized attack on the target in question. “Given CTC’s history, we were invited to review all the articles on the topic in order to compile the discoveries made to date,” Botelho de Souza said.
The review shows that under certain scenarios the combination has been capable of combating cancer in the laboratory and in some patients. “Under others, however, the results weren’t very good. There’s been considerable variability,” Botelho de Souza said.
One possibility in the research conducted at CTC on both solid tumors and blood cancer is to construct CAR T-cells with different receptors and co-stimulators, which could control the disease via different pathways. “We’re also evaluating the effect of removing receptors from cells affected by cancer checkpoints,” he said.
In clinical data, for example, it can be seen that the organism of patients who respond best to treatment with CAR T-cells exhibits higher levels of interleukins 17 and 23. CTC’s scientists have used this information to reprogram T-cells so as to stimulate production of these two interleukins. “In laboratory studies, the results are promising,” Botelho de Souza said.
“One of the challenges of combining multiple editions of CAR T-cells is preventing the immune system from becoming aggressive toward the patient,” Cunha said. In both the product approved by ANVISA and the product to be used in CTC’s clinical trials, the CAR T-cells include a personalized receptor and a co-stimulator protein. “These are second-generation CAR T-cells,” he said.
Cunha is the coordinator of a consensus in the Brazilian Hematology, Hemotherapy and Cellular Therapy Association (ABHH) that is concentrating on the use of CAR T-cells in Brazil. “We’ve established principles for prescribing the treatment, controlling side effects and producing the cells, among other things. This shows Brazil has the maturity necessary to receive this type of technology and try to make it more affordable,” he said.
Universal treatment
CAR T-cell therapy must use T-cells donated by the patient, whose organism would reject cells from anyone else. Sophisticated infrastructure is required to collect cells, transport them safely, manipulate them, and re-infuse them. “The entire procedure, from identifying suitable patients to administering the treatment, can take between 40 and 60 days. The patient may not have that long,” Cunha said.
To make the treatment more affordable and practicable, researchers around the world are investigating genetic modifications to make CAR T-cells “universal”. The goal is for a single line of T-cells to give rise to CAR T-cells for different patients.
Another possibility in trials to reach a universal treatment would be to use a different kind of defense cell. Instead of engineering CAR T-cells, scientists would perform genetic editing of natural killer (NK) cells, which do not have this problem of incompatibility. The method is known as CAR NK-cell therapy. “It’s practicable and also appears to produce a safer inflammatory profile, with less intense side effects,” Botelho de Souza said.
A CTC group led by Virginia Picanço-Castro, a professor at FMRP-USP, is developing different CAR NK-cells to see which ones have the most potential, and has published a review article on promising research results in the field. “Little research involving humans is being done right now, but it’s a matter of time,” Botelho de Souza said.
A drawback of CAR NK-cells is that they do not remain in the organism for very long, he noted. Unlike CAR T-cells, they disappear quickly, and this could hinder long-term control of the cancer. Furthermore, NK cell proliferation and conservation in the laboratory is particularly challenging.
CTC is a Research, Innovation and Dissemination Center (RIDC) supported by FAPESP. It currently has five projects that involve CAR T-cells and CAR NK-cells with funding from FAPESP (19/18702-8, 20/02043-2, 20/14808-3, 20/11413-8, and 21/09900-0).
Source: https://agencia.fapesp.br/39048