

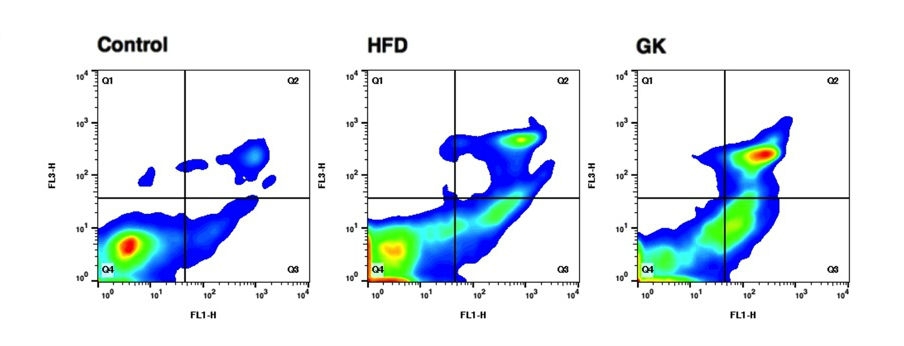
A study published in Scientific Reports identifies changes to neutrophils that appear to explain why people suffering from obesity and type 2 diabetes are more likely to contract infectious diseases (image: cell viability and phosphatidylserine externalization in neutrophils collected from the bronchoalveolar lavage performed in control rats, rats submitted to high-fat diet (HFD) and Goto-Kakizaki (GK) rats. The Q4 region corresponds to cells with intact plasma membrane; in the Q3 regi
Published on 05/13/2021
By Peter Moon | Agência FAPESP – People who suffer from obesity and type 2 diabetes are more likely to become victims of infectious diseases. Both conditions affect the immune system and hence increase the risk of infections. Scientists have long sought a deeper understanding of the mechanism underlying this weakness in the immune system of obese and diabetic individuals.
A study performed at the University of São Paulo’s Biomedical Science Institute (ICB-USP) in Brazil has now demonstrated that the propensity of people with obesity and type 2 diabetes to contract infectious diseases is associated with alterations to neutrophils, which are white blood cells that are part of the immune system and inflammatory response and the first cells to react to the presence of an invasive pathogen in the organism.
Findings from the study have just been published in Scientific Reports, an online journal owned by Springer Nature. The study resulted from the doctoral research of biochemist Wilson Mitsuo Tatagiba Kuwabara and was supervised by biologist Tatiana Carolina Alba-Loureiro, currently at Southern Cross University (UNICSUL).
The study was conducted at ICB-USP in the laboratory formerly led by Professor Rui Curi, currently at Butantan Institute and UNICSUL.
“Kuwabara’s research is highly important because it shows that the conditions for insulin resistance, which we call metabolic syndrome, are associated with a major alteration to neutrophils. It also suggests this alteration may explain the susceptibility of obese people and diabetic individuals to infectious processes,” Curi said.
Kuwabara recalled that the mechanism that makes obese people and diabetic individuals more vulnerable to severe infectious diseases has always been poorly understood. “We found the answer by investigating what happens in neutrophils to transmembrane protein and toll-like receptor TLR4 when it recognizes the toxin LPS in invading pathogens,” he said.
Toll-like receptors (TLRs) are a family of proteins that play a key role in the innate immune system. Impaired activation of TLR4 is a mechanism that can weaken the capacity of immune cells to combat pathogens.
“TLR4 is a membrane receptor and is found in the external membrane of most cells in the organism, but its main role takes place in immune cells. When TLR4 makes contact with invading pathogens, it triggers an immune response by the organism,” Kuwabara said.
TLR4 is activated when it comes into contact with gram-negative bacteria. More specifically, TLR4 activation occurs when the receptor detects a toxin called lipopolysaccharide (LPS) in the external membrane of gram-negative bacteria. When this happens, TLR4 tells the organism to produce more inflammatory substances to combat the invading pathogens. LPS is a soluble endotoxin and can also be found in the bloodstream of infected individuals.
Gram-negative bacteria are among the main causes of severe infectious diseases such as chlamydia, brucellosis, salmonellosis, meningitis, cholera, syphilis and bubonic plague, among others.
The study is part of the regular grant project “The role of neutrophils in the inflammatory response during type 2 diabetes mellitus: cellular and molecular mechanisms”, for which Alba-Loureiro is principal investigator, and is associated with the Thematic Project “Cellular and molecular mechanisms of insulin resistance and inflammation in obese Wistar rats and lean Goto-Kakizaki rats: causes and associations with diet and physical exercise”, for which Curi is principal investigator.
Kuwabara is currently a postdoctoral researcher at ICB-USP, with a scholarship from FAPESP. His research is supervised by Professor José Cipolla Neto.
Experimental models
To understand the TLR4 activation mechanism in obese people and diabetic individuals, Kuwabara performed experiments using two different experimental models with Goto-Kakizaki (GK) and Wistar rats.
The GK rat is a Wistar substrain developed in Japan in the 1970s for the study of diabetes. It spontaneously displays all the classic symptoms of type 2 diabetes, such as insulin resistance, fasting hyperglycemia, hyperinsulinemia, and increased levels of triglycerides and cholesterol in the blood. These rats were especially imported for the experiment at ICB-USP and are the only GK rats in Brazil.
The second model used in the study involved Wistar rats, one of the most commonly used rat strains in scientific studies. In this case, they were fed a high-fat diet (60% of calories from fat) or a control diet for eight weeks. At least eight animals were used in each model.
After eight weeks on the high-fat diet, the Wistar rats exhibited obesity, with liver fat accumulation, glucose intolerance, insulin resistance and inflammation.
To evaluate the neutrophil response to LPS, LPS intratracheal instillation was performed on rats in the models for obesity and type 2 diabetes. A cannula was inserted into the trachea, and LPS in solution was injected directly into the airways.
After six hours, the rats were euthanized to determine the immune system’s response to LPS installation in each group. Blood samples were taken, and bronchoalveolar lavage was performed to collect neutrophils from the inflammatory environment.
To analyze the immune response to LPS, neutrophils isolated from the lavage were counted, cytokine and chemokine volumes were measured, and the activity of myeloperoxidase (MPO), an enzyme used as a neutrophil marker, was evaluated.
The researchers found that LPS intratracheal instillation promoted neutrophil migration to the lungs. The number of neutrophils collected in the bronchoalveolar lavage was smaller in the obese rats and GK rats than in the control group. Similarly, the obese rats and GK rats exhibited less MPO activity and lower production of pro-inflammatory cytokines than the control group.
“After LPS stimulation, we observed less viability in neutrophils collected from GK rats. Compared with the control group, blood neutrophils from GK rats showed a higher death rate in terms of cell membrane integrity loss and increased levels of cleaved caspase-3, a protein that plays a key role in cell death,” Kuwabara said.
“With regard to the obese rats, we found their neutrophils to be more susceptible to cell death even while circulating in the blood and hence before migrating to the lungs to combat the inflammation induced by LPS instillation.”
The data showed that the neutrophil response of GK and obese rats to LPS was impaired, Kuwabara added. In other words, they were LPS-tolerant. “This tolerance may explain the higher death rates in obese patients and diabetic individuals as a result of bacterial infection,” he said.
Biochemical reason
According to Curi, the study is important because it succeeded in demonstrating that neutrophils were involved in an augmented inflammatory process in obese and diabetic rats.
“Thus, when the neutrophils come into contact with bacteria, they’re unable to respond effectively to these agents. This is how the infectious process is installed,” he said.
TLR4 is an essential receptor to the innate immune response, and loss of its activation jeopardizes the inflammatory process and the response to infection.
“Now we know the biochemical reason why obese people and diabetic individuals are more likely to develop diseases. Further research is necessary to find out why TLR4 is inactivated in neutrophils, as described,” Curi said.
The article “Obesity and type 2 diabetes mellitus induce lipopolysaccharide tolerance in rat neutrophils” (doi: https://doi.org/10.1038/s41598-018-35809-2) by Wilson Mitsuo Tatagiba Kuwabara, Caroline Naomi Fukusawa Yokota, Rui Curi and Tatiana Carolina Alba-Loureiro can be read at: www.nature.com/articles/s41598-018-35809-2.
Source: https://agencia.fapesp.br/29891