

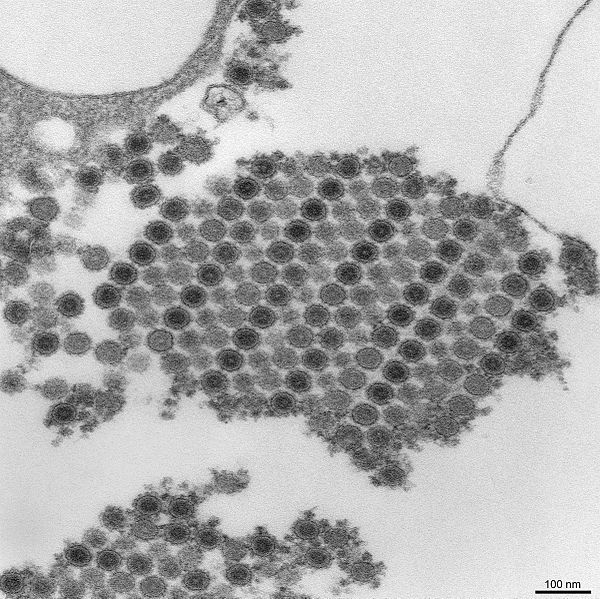
Investigation conducted by international group of researchers showed that chikungunya virus can cause neurological infections. Risk of death in subacute phase is higher for patients with diabetes and significant for young adults (image: Wikimedia Commons)
Published on 03/16/2021
By Maria Fernanda Ziegler | Agência FAPESP – A study conducted by an international team of researchers with FAPESP’s support shows that infection by chikungunya virus can produce even more severe manifestations than the typical symptoms of the disease, such as acute fever, headache, rash, and intense joint and muscle pain.
The analysis was performed by 38 researchers affiliated with the Federal University of Ceará (UFC), the University of São Paulo (USP) and the Ministry of Health in Brazil, and with Imperial College London and Oxford University in the United Kingdom.
Their main discovery was that chikungunya can infect the central nervous system and impair cognitive and motor functions.
“The study produced important new knowledge about the disease and the virus. We not only confirmed that the virus can infect the central nervous system but also found the disease to be more deadly for young adults, rather than children and the elderly as is usually predicted in outbreaks of the disease,” said William Marciel de Souza, co-author of an article on the study published in Clinical Infectious Diseases.
Souza is a researcher at the University of São Paulo’s Ribeirão Preto Medical School (FMRP-USP). “The study also showed that during the acute or subacute phase of the disease [20-90 days after infection] patients with diabetes appear to die seven times more frequently than non-diabetics,” he said.
The study was conducted under the auspices of the Brazil-UK Center for Arbovirus Discovery, Diagnosis, Genomics and Epidemiology (CADDE). It also derived from Souza’s postdoctoral research, part of which he pursued at Oxford University in the UK with FAPESP’s support via a Research Internship Abroad. Researchers affiliated with several different institutions collaborated on the project, which was also supported by Brazil’s National Council for Scientific and Technological Development (CNPq).
Worst outbreak in the Americas
The study was based on a retrospective analysis of clinical and epidemiological data as well as blood, cerebrospinal fluid, and tissue samples from patients who died during the 2017 outbreak in the state of Ceará, Brazil, the worst chikungunya outbreak in the Americas. Ceará notified 194 chikungunya-related deaths and 105,229 suspected cases (1,166 per 100,000 inhabitants) in 2017.
The researchers used documentation filed during the outbreak by the Ceará State Health Department’s Death Verification Service. To ascertain the cause of death in 100 cases, they analyzed blood serum and cerebrospinal fluid samples using the RT-PCR and MinION genome sequencing techniques, immunohistochemistry, and ELISA assays to detect antibodies against chikungunya.
The virus is transmitted by females of two mosquito species, Aedes aegypti and Aedes albopictus. Most chikungunya patients manifest acute symptoms such as high fever, headache, joint and muscle pain, nausea, fatigue, and rash for three weeks after being infected. Some then progress to the subacute phase, during which the symptoms persist. Joint pain may last more than three months, indicating a transition to the chronic phase, which can last years.
All the evidence gleaned from the laboratory tests and clinical records showed that in most cases of suspected death from chikungunya the patient had a central nervous system infection.
“Joint pain was the most frequent symptom, as evidenced by the name of the disease, which refers to contortion from pain [in the East-African Kimakonde language], but we also identified severe problems in the nervous system due to chikungunya,” Souza said.
Viral RNA was found in cerebrospinal fluid from 36 patients and in four brain tissue samples. “The presence of the virus in the brain tissue of those infected is clear evidence that it’s capable of crossing the blood-brain barrier that protects the central nervous system, and of causing infection in the brain and spinal cord,” Souza said.
Most vulnerable
Besides new characteristics of infection by this virus, the researchers also discovered that the risk of death in the subacute phase was seven times greater for patients with diabetes than patients without diabetes.
Their autopsy and histopathological analysis of fatal cases pointed to viral infection as the cause of bloodstream disorders and fluid imbalances in the brain, heart, lungs, kidneys, spleen, and liver.
“The study confirmed some previous clinical findings about death from chikungunya and also brought up novel aspects of the disease and its lethality. This new information, obtained in a painstaking analysis of the Ceará outbreak, will contribute to the recognition of the factors that cause severity and also to further research to develop better treatments in future,” said Luiz Tadeu Moraes Figueiredo, a professor at FMRP-USP and also a co-author of the article.
Figueiredo is engaged in research supported by FAPESP on high-throughput sequencing (HTS) to identify and characterize viruses without requiring viral isolation or cell culture. He is particularly interested in MinION genome sequencing, which is faster and more affordable than other approaches. The technology also reads RNA and DNA in real time and in a single stage.
Based on their analysis, the authors of the study concluded that older people and children were not at greater risk of dying from chikungunya than other age groups, in contrast with the profile typical of arbovirus epidemics. In the 2017 outbreak, most of the fatal victims were middle-aged.
“We normally associate arboviruses with hospitalizations and deaths for elderly patients and infected children, but our analysis of these 100 fatal cases showed that a majority [over 60%] of those with infection in the central nervous system were adults aged 40 or more,” Souza said, adding that patients aged anywhere from 3 days to 85 years were among the rest of the fatal victims.
The findings show that defective or suppressed immunity is not necessarily the main source of susceptibility to the disease in such outbreaks. “Many of the victims were healthy young adults under 40, and most had no comorbidities,” he said. “The analysis added another layer to our knowledge of the disease and can be extremely important to clinical practice. Even greater attention should be paid to this age group, which is also at great risk of dying.”
The article “Fatal outcome of chikungunya virus infection in Brazil” (doi: 10.1093/cid/ciaa1038) can be read at: academic.oup.com/cid/advance-article/doi/10.1093/cid/ciaa1038/5885158.
Source: https://agencia.fapesp.br/34514