

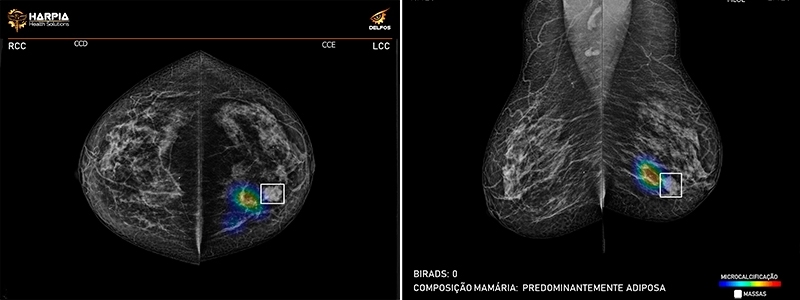
A startup supported by FAPESP has developed a technology based on artificial intelligence that can reduce the time to produce a diagnosis by 40% (photo: Harpia)
Published on 07/11/2022
By Fábio De Castro | Agência FAPESP – A startup based in São Paulo state, Brazil, has created an innovative computational method that enables radiologists to work faster and use a simpler and more accurate method of analyzing mammograms to locate suspect breast alterations.
Harpia Health Solutions deployed artificial intelligence resources such as machine learning and neural models to develop its Delfos platform for automatic identification and classification of breast tissue anomalies and lesions in mammograms, facilitating the screening process conducted by radiologists.
Development of the solution by the firm, which is located in the São José dos Campos Technology Park (PqTec), was supported by the FAPESP Innovative Research in Small Business Program (PIPE).
“Mammograms are sent to the cloud, and Delfos returns the results in up to five minutes,” said Daniel Aparecido Vital, the researcher responsible for the project and an equity partner in Harpia.
The Delfos platform is integrated with the picture archiving and communication system (PACS) software used by clinics to view and store mammograms, he explained.
A mammogram is an X-ray picture of the breast. Doctors use mammograms to look for early signs of breast cancer. Early diagnosis through screening mammograms has a greater overall impact on survival rates.
“It’s important for the solution to be integrated with PACS, which is already part of radiologists’ routine. The platform is totally automated and can result in various benefits, such as improved assertiveness, reducing diagnostic inconsistency by up to 15%, up to 40% higher productivity, and an increase of up to 20% in early diagnosis, as well as significant cost savings for operators, hospitals and clinics,” Vital said.
The agility of the new method also helps physicians make better decisions in priority queuing, as well as expediting issuance of diagnostic exam reports. The technology automatically indicates the presence of lumps, masses and calcifications, helping the radiologist with patient triage.
“The time taken to produce a diagnosis can be reduced by about 40%. An important factor is that the radiologist isn’t required to perform tasks with low cognitive value, and can focus on analyzing suspicious findings,” Vital said.
High tech
The firm was established in April 2019 at Nexus incubator in PqTec by a group of students, former students and professors of biomedical engineering at the Federal University of São Paulo’s Science and Technology Institute (ICT-UNIFESP) in São José dos Campos. Vital’s equity partner is Catarina Cardoso Reis, and Professors Henrique Alves de Amorim and Matheus Cardoso Moraes are co-founders and scientific consultants to the firm.
The PIPE project was completed in November 2021, and the solution developed by Harpia is now a commercial product. Delfos processed 35,000 mammograms in 2021. “The number is higher now. We’re processing 12,000-13,000 mammograms per month. We have 12 clients in six states, and we’re negotiating with large companies in the healthcare sector to sign up more partners,” Vital said.
Mammograms without any digital processing may lack crucial information for rapid analysis aimed at diagnosis of breast cancer, he added, and designers of diagnostic support systems have pursued ways to filter medical images for radiologists since the 1990s. However, these systems have limited accuracy and scope.
“We wanted to take a step forward using high tech such as artificial intelligence and computer vision,” Vital said. “Harpia developed all the tools used by Delfos based on existing technologies but with several unique modifications involving neural models, machine learning and deep learning.”
Another important point is that the entire development process and training of the intelligent system was based solely on a diversified sample of mammograms executed in Brazil, representing the highly heterogeneous profile of its population. “Delfos is integrated with the client’s system and distinguishes between lumps and other suspicious findings, providing physicians with an automatic assessment of several features, such as breast density, axillary lymph nodes, symmetry, and calcifications,” Vital said.
Lumps and calcifications are identified visually. “Indication boxes and heat maps are used to display the size and location of suspect structures in breast tissue quadrants. The radiologist can identify the findings at a glance,” he explained.
The solution runs entirely online so that clinics and hospitals do not need to have any related local infrastructure. According to Vital, clients pay per processed exam, per package of exams, or by subscription, in which case extra payment is required if the limit is exceeded. Demand varies considerably, he explained, with some clients processing 100 mammograms per month and others handling as many as 8,000 per month.
Vital said Harpia is partnering with suppliers of PACS to enable integration with Delfos to evolve continuously. “We have a router that’s integrated with clients’ imaging systems. The PACS send exams to us in the cloud automatically,” he explained. As a result, in less than five minutes a complete analysis and diagnostic report is available to the physician who ordered each exam.
“That’s important because the patient may still be at the clinic in that timeframe. Depending on the result, the patient can immediately be examined by ultrasound as a complement, avoiding the need to make another appointment if something suspect is detected,” Vital said.
The next step for Delfos is development of the capability to distinguish between malignant and benign growths. “The system is already capable of separating exams with suspect findings from those without, automating the radiologist’s work and reducing the time taken to reach a diagnosis, but it can’t say whether what’s detected is benign. We want to take this next step in our Phase 2 PIPE project,” Vital said.
Source: https://agencia.fapesp.br/39102