

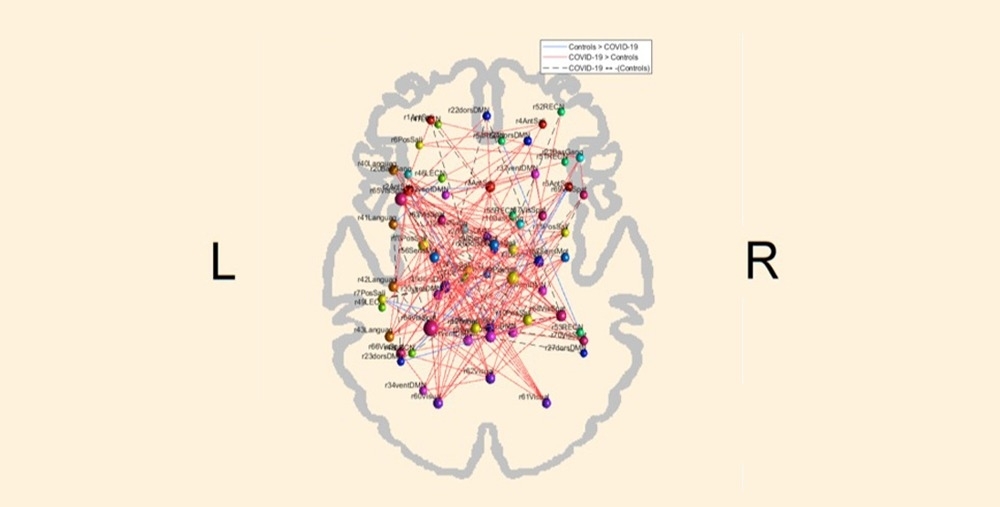
The blue lines in the image represent connections diminished in post-COVID brains compared to the control group. The red lines show connections augmented in participants who had been infected by SARS-CoV-2 (image: Brunno Machado de Campos/UNICAMP)
Published on 03/15/2021
By Karina Toledo | Agência FAPESP – Preliminary findings of a study conducted at the University of Campinas (UNICAMP) suggest that even mild cases of COVID-19 can alter the brain’s functional connectivity pattern, causing a kind of synaptic “short circuit”.
The findings are based on a comparison of functional magnetic resonance imaging (fMRI) scans performed with a rest sequence on 86 volunteers who had recovered from the disease at least two months previously, and scans on a control group of 125 subjects who had never contracted the disease.
“In a normal brain, certain areas are synchronized during an activity, while others are at rest. In these subjects who had COVID-19, we observed a severe loss of brain network specificity. Everything’s connected at the same time. This probably leads to an increase in energy expenditure by the brain, which nevertheless becomes less efficient,” said Clarissa Yasuda, a neurologist, professor at UNICAMP’s Medical School (FCM-UNICAMP) and member of the Brazilian Research Institute for Neuroscience and Neurotechnology (BRAINN), one of the Research, Innovation and Dissemination Centers (RIDCs) funded by FAPESP.
Yasuda presented the findings, which have not yet been published, on January 27 during the 7th BRAINN Congress. The study is still in progress, and the group plan to include more participants, tracking the complications caused by the novel coronavirus to the central nervous system for at least three years.
According to Yasuda, exactly how the virus alters brain connectivity is unknown, but some theories are worth investigating. “It’s possible that infection by the virus damages the synapses in certain neuronal circuits, and to compensate for the resulting signal failure the brain activates other networks simultaneously,” she told Agência FAPESP. “This hyperconnectivity may also be an attempt by the brain to restore communication in the affected areas.”
Another possible explanation to be tested by the group is that cerebral dysfunction lies behind some of the longer-term complications of COVID-19 reported by many patients, such as fatigue, daytime sleepiness, memory loss, and confusion (“brain fog”).
“We plan to compare brain function in patients with these long COVID symptoms and patients who make a full recovery without post-COVID syndrome,” Yasuda said. “If our research bears out the correlation between hyperconnectivity and persistent neuropsychological symptoms, we may think about drugs and other kinds of treatment for the problem.”
Structural and functional alterations
Work on the project began in the second half of 2020 with an online questionnaire completed by more than 2,000 people in all regions of Brazil. Only individuals diagnosed with the disease by RT-PCR were eligible. Around 90% did not require hospitalization and were treated at home. In this phase, the participants reported the symptoms experienced about two months after they were diagnosed. The most common were fatigue (53.5%), headache (40.3%), and memory loss (37%).
After six months, 642 respondents to another online survey reported long-term complications such as fatigue (59.5%), daytime sleepiness (36.3%), memory loss (54.2%), difficulty concentrating (47%), and impairment of routine activities (23.5%). In addition, symptoms of anxiety were reported by 41.9%, well above the average for the Brazilian population, which is about 10%.
Some of the volunteers were physically examined by the researchers, given neuropsychological tests to assess cognitive functions such as memory and attention, and submitted to fMRI brain scans for analysis of gray matter (containing neuronal cell bodies) and white matter (axons and glial cells). These assessments were performed when the acute phase had ended, on average 55 days after diagnosis.
“We adjusted the results of the neuropsychological tests for age, sex, and educational attainment,” Yasuda said. “Subjects with long COVID syndrome performed much worse than expected in cognitive terms, indeed worse than the Brazilian average for some tasks.”
The fMRI scans showed that some volunteers had decreased cortical thickness in some brain regions compared with the average for controls, including areas relating to anxiety. Cortical thickness was increased in others, possibly due to swelling as a result of the infection (read more at: agencia.fapesp.br/34404/).
More recently, using a technique called tractography, the researchers found lesions in the white matter microstructure but the implications are as yet unknown. Tracts are neural pathways in the central nervous system.
“No one really knows exactly how the virus affects the brain, whether the damage is indirect, resulting somehow from inflammation, or directly due to infection of brain cells,” Yasuda said. “In any event, the findings are surprising and a little alarming. I think it’s very clear that COVID-19 is much more dangerous than flu.”
Source: https://agencia.fapesp.br/35152