

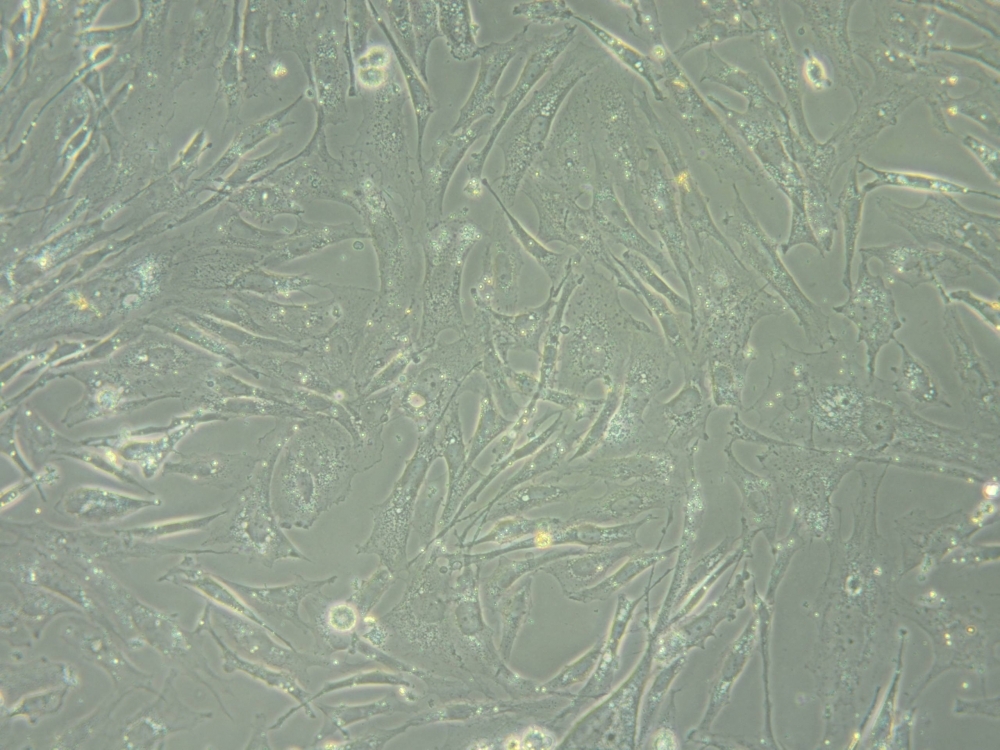
A study conducted by researchers at the Center for Cell-Based Therapy in São Paulo state, Brazil, identified a genetic signature that can be used to predict whether patients should be submitted to radiation therapy (image: CTC).
Published on 08/20/2021
By Maria Fernanda Ziegler | Agência FAPESP – Researchers at the Center for Cell-Based Therapy (CTC) have discovered a set of biomarkers that can be used to predict which patients diagnosed with glioblastoma, an aggressive form of brain cancer, may have tumors that are more resistant to radiation therapy. The discovery, published in the journal Frontiers in Oncology, can help doctors choose the treatment that should enable patients to live longer.
Gliomas are graded on a scale of one to four. Grade four gliomas are the most aggressive and are also known as glioblastoma. Glioblastoma is the most common and aggressive malignant primary brain tumor in adults. It usually has to be surgically removed, followed by chemotherapy or radiation therapy, or both, to eliminate what could not be surgically removed and ensure the tumor does not return. However, patient survival tends to be low owing to the tumor’s resistance to treatment. According to most estimates, 80% of patients submitted to radiation therapy suffer a relapse a few months later.
“Our study provides important information for use in screening patients prior to deciding whether radiation therapy should be used. It’s a large signature. We identified 31 genes that may indicate resistance or sensitivity to radiation when altered. So it’s possible to verify whether there are tumor cells that are highly resistant to radiation, potentially assisting physicians in deciding on the optimal treatment,” said Valéria Valente, a professor at São Paulo State University’s School of Pharmaceutical Sciences (FCF-UNESP) in Araraquara and a researcher affiliated with CTC, one of the Research, Innovation and Dissemination Centers (RIDCs) supported by FAPESP.
The study was also funded directly by FAPESP via a Regular Research Grant.
To arrive at the biomarker panel, the researchers first analyzed gene expression profiles in glioblastoma cell lines, having already found that resistance to treatment varied depending on cell lineage. They then analyzed the transcriptomes using RNA sequencing to identify the genes expressed by tumor cells and the gene expression patterns associated with sensitivity or resistance to radiation therapy. They confirmed the results of these laboratory analyses by cross-tabulating them with data from The Cancer Genome Atlas (TCGA) containing the genomes and clinical information for glioblastoma patients showing sensitivity or resistance to radiation.
“Some lineages are more proliferative, and these are also the most sensitive to radiation. When we correlated that finding with the transcriptome data, we found overall gene expression patterns linked more to one group or another,” Valente said.
Like any type of cancer, gliomas are heterogeneous, she added. This is particularly so in the case of these tumors, which are made up of different cell types, some more radioresistant than others. “The point of this biomarker panel is that it can be used to identify tumors containing cells with the gene expression signature associated with radioresistance,” she said.
The correlations between patient clinical data and the radioresistance signature showed that patients with alterations in at least 21 genes in the panel did not respond well to the treatment. Survival was low whether or not they were irradiated. “That’s an important indication because it shows there are certain individuals who won’t benefit from radiation treatment, which will cause additional suffering and won’t help them live longer,” Valente said.
Which genes?
The genes that form the panel are not associated with a specific function. The researchers found that cell lines with reduced proliferation and more radioresistance displayed alterations in extracellular matrix (ECM) and receptor genes. As they note in the article, the “ECM-receptor pathway is a master regulatory pathway that is known to impact several cellular processes including survival, proliferation, migration, invasion, and DNA damage signaling and repair”.
Cell lines that proliferated more and were more sensitive to radiation had a different signature, with consistent enrichments for DNA repair processes. Another curious finding was that although several ECM-receptor genes were overexpressed in radiosensitive cells, the signaling cascade was faulty and the pathway did not function correctly.
“This is an interesting detail of the study that merits further investigation,” Valente said. “In resistant cells, most of the alterations were paired, meaning that when a gene is altered the receptor for an extracellular protein is augmented and so is the extracellular protein coupled to it, so that the pathway functions. In sensitive cells, the genes for this pathway are also altered, but in a truncated manner, and the connections established in the signaling pathway don’t work. Something is missing, and activation of this route isn’t completed. Each of the pathways we identified needs to be analyzed individually in future research.”
“The idea now is to investigate this phenomenon in other tumors. The findings include important evidence that could augment the arsenal of therapeutic biomarkers applied to cancer and help oncologists recommend the best treatment,” said Wilson Araújo Silva Junior, leader of the CTC group.
The article “Expression profiling of glioblastoma cell lines reveals novel extracellular matrix-receptor genes correlated with the responsiveness of glioma patients to ionizing radiation” (doi: 10.3389/fonc.2021.668090) by Rodolfo Bortolozo Serafim, Patrick da Silva, Cibele Cardoso, Luis Fernando Macedo Di Cristofaro, Renato Petitto Netto, Rodrigo de Almeida, Geovana Navegante, Camila Baldin Storti, Juliana Ferreira de Sousa, Felipe Canto de Souza, Rodrigo Panepucci, Cristiano Gallina Moreira, Larissa Siqueira Penna, Wilson Araujo Silva Jr and Valeria Valente is at: https://www.frontiersin.org/articles/10.3389/fonc.2021.668090/full.
Source: https://agencia.fapesp.br/36603