

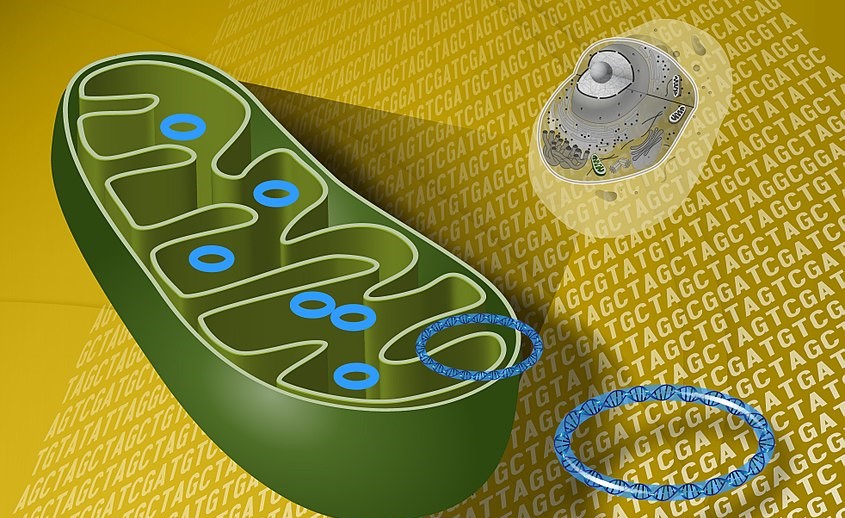
The analyses showed that production of ATP by mitochondria can remain impaired even after the virus has been eliminated from the organism (image: Darryl Leja/NHGRI/Wikimedia Commons)
Published on 12/11/2023
By Maria Fernanda Ziegler | Agência FAPESP – A study by an international team of researchers reported in an article published in Science Translational Medicine shows that SARS-CoV-2, the virus that causes COVID-19, can impair the functioning of mitochondria, the cell’s powerhouse, in vital organs such as the heart, brain, kidneys, liver and lungs, with lasting effects on the entire organism of those infected.
The discovery of a systemic effect that inhibits mitochondrial functioning will help scientists develop novel treatments for severe cases of the disease and long COVID.
“The mitochondrial dysfunction caused by SARS-CoV-2 is conserved even when the virus is eliminated. It’s yet another systemic effect of the disease. In our study, we found that the process occurred in various tissues throughout the organism and not just in immune system cells [such as monocytes] or only in the lungs, as used to be thought. Mitochondrial dysfunction can occur in the entire organism, with consequences that include an exacerbated inflammatory response in severe patients,” said Pedro Moraes-Vieira, one of the co-authors of the article. He is a professor at the State University of Campinas’s Biology Institute (IB-UNICAMP) in Brazil.
The study was conducted by the COVID-19 International Research Team, a consortium of researchers who participate on an individual basis mainly in the United States, South Korea, Denmark, Paraguay and Brazil. Their main source of funding is the US National Institutes of Health (NIH).
This particular study was a continuation of an investigation begun in 2020, with support from FAPESP, in which the UNICAMP group led by Moraes-Vieira first discovered that COVID-19 could cause mitochondrial dysfunction, although they did not find proof that the problem could be systemic (read more at: agencia.fapesp.br/33296).
Stolen energy
In this latest study, the researchers analyzed infection by SARS-CoV-2 using two animal models (hamsters and mice). They also processed data for more than 700 nasopharyngeal samples from healthy people and early-stage COVID-19 patients, and 35 autopsy tissue samples collected during the pandemic in New York City from individuals with late-stage infection.
The analyses showed that the virus suppressed the expression of certain mitochondrial genes (the organelle has its own genetic material – mitochondrial DNA), affecting biochemical pathways, production of cellular energy, and immune response activation. As a result, cells turned to the alternative of glycolysis, a metabolic pathway that breaks down glucose into pyruvate. This acid supplied the virus with energy, which was able to replicate more and triggered the exacerbated inflammatory response typical of severe COVID-19.
The systemic effects of mitochondrial dysfunction did not stop there. “We observed that even when the virus had been eliminated from the organism and mitochondrial gene inhibition in the lungs had ceased, expression of these mitochondrial genes in the heart, kidneys, liver and lymph nodes remained impaired, potentially leading to severe COVID-19. We believe this inhibition of mitochondrial genes may also be linked to long COVID, a condition in which the virus is no longer present. The disease has been cured, but the patient still has some symptoms and sequelae,” said Moraes-Vieira, who is also a member of UNICAMP’s Experimental Medicine Research Cluster (EMRC) and of the Obesity and Comorbidities Research Center (OCRC), a Research, Innovation and Dissemination Center (RIDC) supported by FAPESP at UNICAMP.
As Moraes-Vieira, experiments involving infected monocytes conducted by the UNICAMP group in 2020 showed that suppression of mitochondrial genes almost completely inactivated oxidative phosphorylation, which uses the energy released by nutrient oxidation to produce a key fuel for cells called adenosine triphosphate (ATP).
“This creates a need to seek other ways of producing energy, potentially leading to the shortness of breath and fatigue that are symptoms of long COVID, among others,” he explained. This finding was published in 2020 by Moraes-Vieira and his group.
Analysis of the nasopharyngeal swabs and tissue samples in the latest study showed that suppression of mitochondrial genes and functioning occurred in several organs, such as the heart, liver, kidneys and lymph nodes.
“Even after elimination of the virus, inhibition of genes associated with oxidative phosphorylation persisted. It appears to be an irreversible condition in cases of long COVID. The findings can help find novel treatments to restore mitochondrial function. We’ll be focusing on exactly that in future research,” he said.
The article “Core mitochondrial genes are down-regulated during SARS-CoV-2 infection of rodent and human hosts” is at: www.science.org/doi/10.1126/scitranslmed.abq1533.
Source: https://agencia.fapesp.br/50440