

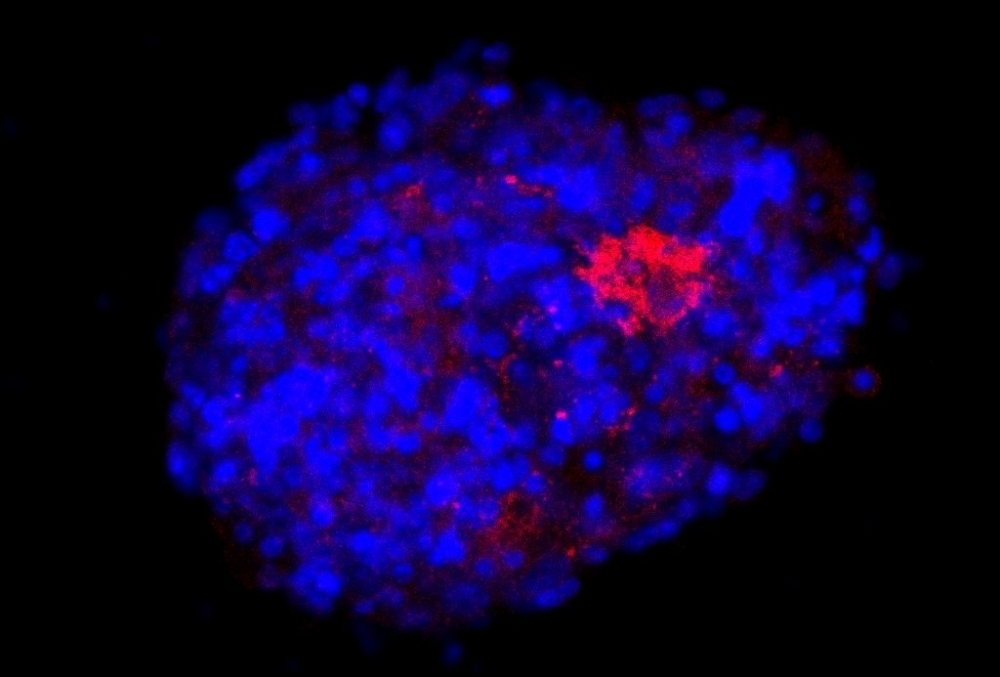
A neurosphere obtained from mouse neural stem cells and infected with an adapted SARS-CoV-2. The image was produced by immunofluorescence, with the cell nucleus and viral spike protein stained blue and red respectively (image: Bruna A. G. de Melo/UNIFESP)
Published on 06/13/2022
By André Julião | Agência FAPESP – Researchers in Brazil affiliated with the Federal University of São Paulo (UNIFESP) have used murine cells to develop a bioprinted three-dimensional model of the brain to study the neurological action of SARS-CoV-2. They have also succeeded in creating an adapted version of the virus that infects murine neural cells. The results of the research are reported in an article published in the journal Advanced Biology. The group expects them to accelerate and reduce the cost of future studies on the effects of COVID-19 on the central nervous system.
“We set out to create 3D bioprinted models that could be used to study the virus’s invasion mechanisms and the action of drugs, among other things. Because the SARS-CoV-2 that infects humans doesn’t infect mice, we used mice that had been genetically modified to express the human receptor [ACE-2, the protein to which the virus binds in order to invade cells]. But we wanted a version of the virus that was adapted specifically for the animals’ neural cells,” said Marimélia Porcionatto, a professor at UNIFESP’s Medical School (EPM) and principal investigator for the project, which is funded by FAPESP.
A team of virologists participated in the project, among them Juliana Maricato and Luiz Mário Janini, both professors at EPM-UNIFESP. Janini is also supported by FAPESP.
The bioink created by the group is a mixture of natural compounds with neural cells fed into a 3D printer. The model was developed in previous projects and enables the cells to survive the bioprinting process, migrate in space, and interact as if they were in living nerve tissue. According to the researchers, they used mouse cells but the materials are biocompatible and can be adapted to human cells in future (more at: agencia.fapesp.br/37839).
“We’ve now added neurons to the model as well as astrocytes. Neurons are more sensitive and were added later as if they were seeded onto the bioprinted material, so they not only integrated into the model but interacted with the astrocytes,” said Bruna Alice Gomes de Melo, first author of the article. The research was conducted while she was a postdoctoral fellow at EPM-UNIFESP.
More types of neural cells can be added in future, increasing the complexity of the model and making it more like neural tissue, the researchers explained.
The group’s other 3D models are organoids and spheroids, clusters of cells that self-organize in laboratory cultures. “Our model is more reproducible than organoids and spheroids. It can also be produced on a larger scale,” Porcionatto said.
Adapted virus
The spheroids – structures formed from neural stem cells and also known as neurospheres – were crucial to developing the version of SARS-CoV-2 adapted for use in mice. This entailed incubation for seven days with particles of the viral strain that infects humans. The few particles that survived and replicated were then isolated and placed in a new culture of neurospheres. The process was repeated four times to produce a sufficient quantity of viruses for the requirements of the trials.
Genetic sequencing of the resulting virus showed that it had shed some of the mutations found in the strain used in the first stage of incubation. The adapted coronavirus was also more similar to the Wuhan strain that started the pandemic.
Vero cells normally used as a model for infection in humans were submitted both to the wild-type and adapted viruses. The latter’s capacity to infect cells other than those from mice was found to be low.
An interesting result obtained with the bioprinted 3D model was that the adapted virus replicated 30 times more efficiently in astrocytes than in neurons, demonstrating the importance of the former to central nervous system infection by SARS-CoV-2.
“The pathogen can be simply present in cells without replicating enough to cause problems for the organism. The results showed that viral particles were reproducing and exiting cells to invade others and keep spreading the infection,” Melo said.
In addition, during the infection, the researchers observed increased expression of chemokines, molecules that attract immune system cells. The increase led to a reduction in the number of inflammatory cytokines.
“This means our model reproduces what would happen in the organism and is an improvement on organoids and spheroids, let alone cells on two-dimensional slides,” Porcionatto said. “Furthermore, other cells that appear to be involved in infection of the brain by SARS-CoV-2 can be added to the bioink we developed, such as microglia and endothelial cells in the blood-brain barrier lining the inner walls of blood vessels in the brain.”
The researchers expect the model to reduce the cost of this kind of research and the use of laboratory animals.
The research was supported by FAPESP via three other projects (18/12605-8, 19/01255-9, and 21/03684-4).
The article “3D bioprinted neural-like tissue as a platform to study neurotropism of mouse-adapted SARS-CoV-2” is at: onlinelibrary.wiley.com/doi/10.1002/adbi.202200002.
Source: https://agencia.fapesp.br/38867