

Electron cryomicroscopy of chikungunya virus, which has been endemic in Brazil for more than a decade (image: NIH 3D)
Published on 03/12/2024
By Julia Moióli | Agência FAPESP – The chikungunya virus, transmitted by Aedes aegypti and Aedes albopictus mosquitoes and responsible for more than 900 deaths in Brazil since it arrived around ten years ago, is capable of spreading through the blood, reaching multiple organs and crossing the blood-brain barrier, which protects the central nervous system. The mechanisms of action observed for the first time in fatal cases by a group of Brazilian, American and British researchers were reported in an article published on March 12 in the journal Cell Host & Microbe. The findings reinforce the need to update treatment and surveillance protocols.
With more than 10 million cases recorded in around 125 countries over the past 20 years, including 2 million in Brazil alone, where it has been endemic for more than a decade, the disease caused by the chikungunya virus (CHIKV) is still mistakenly considered to be less deadly than dengue. To help dispel this myth, researchers from the State University of Campinas (Unicamp), the University of São Paulo (USP) and the Central Public Health Laboratory of Ceará (Lacen) in Brazil, the University of Kentucky and the Texas Medical Branch in the United States, and Imperial College London in the United Kingdom conducted the most comprehensive analysis to date on the subject. Last year, the group reported the high lethality of CHIKV in Ceará, the state with the highest number of cases in Brazil.
The study, funded by FAPESP (projects 17/25588-1, 17/13981-0, 18/14389-0, 19/00098-7, 19/24251-9 and 19/27333-6), analyzed data from 32 deceased patients. It included test results for the presence of CHIKV in the body, as well as laboratory and autopsy information. The following were performed in samples of blood serum, cerebrospinal fluid and other tissues: histopathology (a technique that consists of analyzing paraffin-fixed tissues under a microscope), quantification of cytokines (signaling proteins secreted by defense cells), metabolomics (analysis of the set of metabolites present in the serum), proteomics (set of proteins) and viral genomic analysis, as well as real-time reverse transcription-polymerase chain reaction (RT-qPCR), a laboratory technique that allows the early detection and quantification of viruses based on their genetic material.
For comparison purposes, the scientists also evaluated samples and tests from two other groups, one consisting of 39 survivors of acute CHIKV infection and the other consisting of 15 blood donors (adults with no infection and presumed to be healthy).
Central nervous system invasion
One of the findings that most caught the researchers’ attention was the presence of CHIKV in cerebrospinal fluid samples, indicating its ability to cross the blood-brain barrier, the physical layer that protects the central nervous system and normally prevents pathogens from entering.
According to the article, this “invasion” occurs through two mechanisms: first, the virus infects CD14+CD16+ monocytes (defense cells that have CD14 and CD16 molecules on their surface) and, in the presence of high levels of CCL-2 (an inflammation-regulating protein that is part of the immune system), migrates across the barrier and is transported to the brain; second, the infection affects proteins that are important for holding the epithelial cells of the blood-brain barrier together.
“This shows that CHIKV is not only responsible for arthralgia [joint pain], which causes fever, muscle pain and joint swelling, but leads to neurological damage,” explains William Marciel de Souza, professor at the University of Kentucky (United States) and lead author of the study.
“In the blood, we observed a severe alteration in the coagulation cascade, with a decrease in some key proteins, as well as hemodynamic damage in the organs, i.e. excess fluid. In the immune system, the levels of cytokines associated with inflammation were higher than those observed in chikungunya patients who survived.”
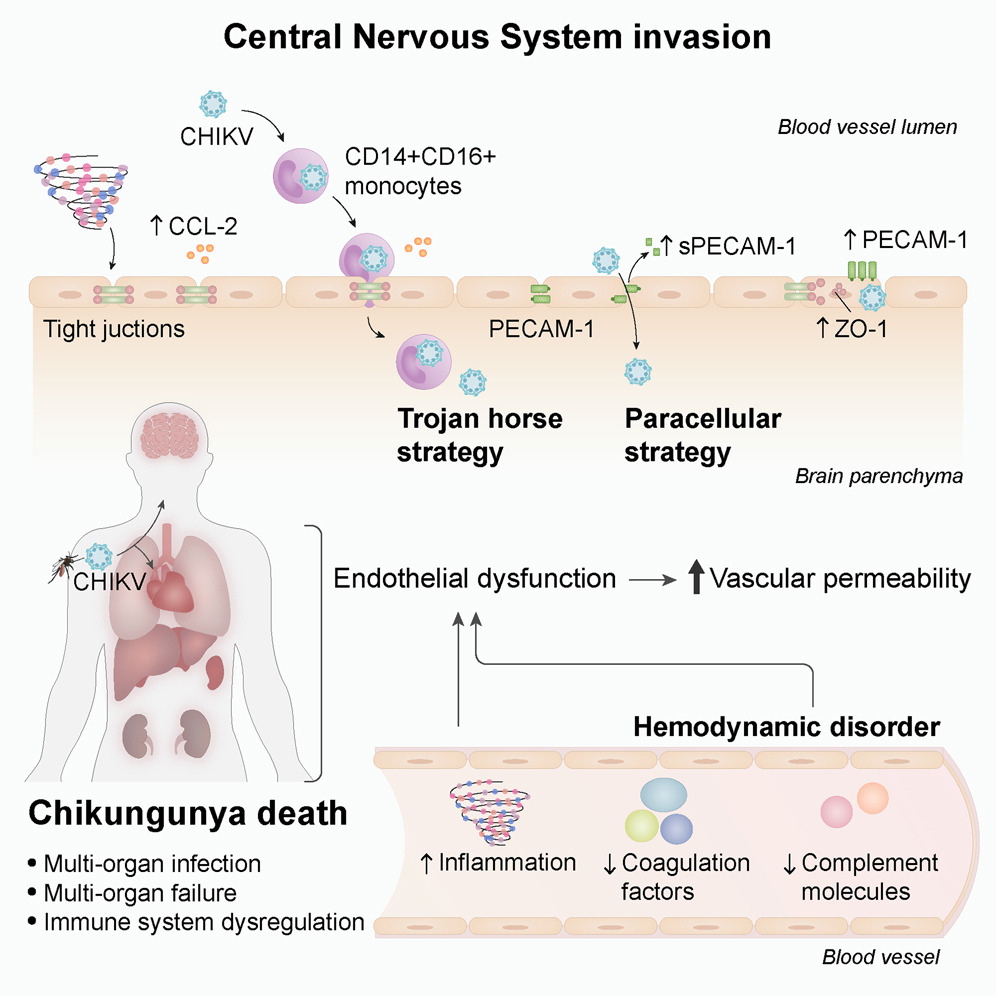
Graphic summarization of the article’s main findings (image: Cell Host & Microbe)
Public health
Understanding the biological mechanisms of any disease contributes to the development of effective treatments, prognostic biomarkers and clinical management strategies. According to the researchers involved in the work, this is fundamental in the case of chikungunya for two reasons:
“There are still no large-scale immunization programs – the first vaccine against the virus was approved by the Food and Drug Administration [US health surveillance agency] last November – and outbreaks are likely to continue following the same pattern in Brazil, i.e. affecting many people at once, but in small geographical pockets,” says José Luiz Proença Módena, a professor at UNICAMP’s Institute of Biology. “Public health teams need to be prepared for this, including genomic, serologic and ICU [intensive care unit] surveillance.”
“In addition, heart failure and neurological conditions are not traditionally associated with the disease, but in a fraction of the population affected by this virus, they can occur and leave sequelae or even lead to death,” adds Souza.
The research was also supported by the Brazilian National Council for Scientific and Technological Development (CNPq), the Brazilian Ministry of Science, Technology and Innovation (MCTI), the National Institutes of Health (NIH), the Burroughs Wellcome Fund, the Bill & Melinda Gates Foundation, the Wellcome Trust and the Global Virus Network.
The article “Pathophysiology of chikungunya virus infection associated with fatal outcomes” can be read at: www.cell.com/cell-host-microbe/fulltext/S1931-3128(24)00054-4.
Source: https://agencia.fapesp.br/51084