

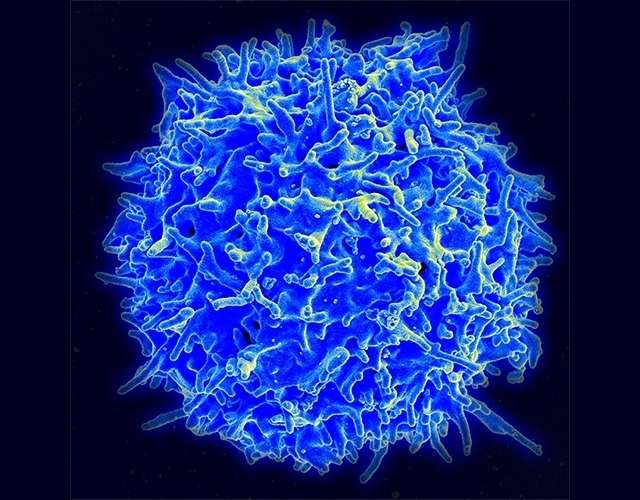
Present in the most aggressive cases of a disease known as SPTCL and accounting for 60% of all cases, these mutations make the immune system attack the organism instead of protecting it (scanning electron microscope image of a healthy human T lymphocyte / image: NIAID)
Published on 05/13/2021
By André Julião | Agência FAPESP – An international group of researchers including Brazilians has identified two genetic mutations that appear to account for 60% of cases of subcutaneous panniculitis-like T cell lymphoma (SPTCL), a rare form of skin cancer.
Mutations in a gene encoding a checkpoint protein that modulates the immune system are present in the most aggressive cases of the disease. The study, published in Nature Genetics, is the first to link the cause of a disease to alterations in a checkpoint protein.
Checkpoints are molecular circuits that ensure the proper timing of cell division, and they involve a set of proteins that monitor cell growth and DNA integrity. Uncontrolled propagation of damaged DNA can contribute to tumorigenesis.
Pharmacological targeting of checkpoints is considered the most promising advance in cancer treatment for several decades. However, the discovery that a mutation in this type of gene can cause rather than treat disease serves as a warning about the possible risks of using drugs to modulate checkpoints.
SPTCL is a type of non-Hodgkin lymphoma that evolves slowly in most cases. The main symptoms are red skin bumps similar to those caused by panniculitis (inflammation of subcutaneous adipose tissue) and lupus, prolonged fever, and swelling of the liver and spleen. It is often misdiagnosed because of these similarities to other conditions, delaying appropriate treatment.
“It’s the first disease described in humans linked to the lack of normal expression of a checkpoint protein not caused by a drug but by genetic factors,” said Elvis Valera, a staff physician at the general hospital of the University of São Paulo’s Ribeirão Preto Medical School (HC-FMRP-USP) in Brazil and a professor of graduate studies in the institution’s Child and Adolescent Health Program.
Valera is the only Brazilian researcher involved in the study, which has more than 40 authors affiliated with institutions in Australia, Canada, France and French Polynesia. The study was conducted while he was working at McGill University in Montreal, Canada, with FAPESP’s support. His research was supervised by Professor Nada Jabado.
The checkpoint protein involved in the disease studied by the group is TIM-3 (T cell immunoglobulin mucin 3), a protein that modulates the immune response and is encoded by the gene HAVCR2 (hepatitis A virus cellular receptor 2). Like other checkpoint proteins, it identifies what belongs to the organism and what is invasive in order to determine targets to be combated by the immune system. When a checkpoint protein is inactivated, the immune system of an organism attacks components that should be identified as belonging to that organism.
The two mutations in question, which were found in 16 out of 26 DNA samples from patients with SPTCL, lead to a TIM-3 deficiency, which dysregulates the immune system. In this study, the Y82C mutation was more frequent in patients of East Asian and Polynesian origin, while the I97M mutation was found mainly in patients of European origin.
Siblings
Valera conducted the research in parallel with the work that originally took him to McGill, in which he measured biomarkers in the spinal fluid, blood and urine from children with brain cancer. Shortly before his arrival in Canada, his supervisor Jabado, also a pediatric oncologist, had seen three siblings of East Asian origin. Two had SPTCL, while the third did not. Jabado took the opportunity to sequence the DNA of all three siblings and their parents, who had not manifested the disease.
“This was what we call a family cluster. Because SPTCL accounts for less than 1% of non-Hodgkin lymphomas in children, it was a unique opportunity. After DNA sequencing, we began analyzing the genes that could correspond to a heritability pattern,” Valera explained.
The researchers drew up a long list of candidate genes, aiming to identify their function and whether they were associated with the disease. TIM-3 drew their attention because it is known to be linked to T cells, a type of lymphocyte that plays a central role in cell-mediated immunity and hence could be linked to SPTCL.
Jabado contacted researchers in France, who established a small hospital consortium to collect more samples for comparison. The study was later joined by researchers in Australia and French Polynesia to provide a broader cross-section of DNA samples in addition to those collected in France and Canada.
“Having brought together the 26 DNA samples, they found similar alterations in some well-conserved alleles across several individuals,” Valera said. “This suggested a founder effect, a random allele change inherited from a common ancestor. It was particularly evident in the patients of East Asian origin, including in the first family, who gave rise to the study.”
Next, the researchers noticed another predominant mutation in the samples from patients of European origin. “Although they were different, the mutations were very close to each other in the TIM-3 protein, so we suspected their effects would be similar,” Valera said.
Approximately 60% of the samples had one of the two mutations, and the researchers concluded that the mutations probably caused the disease. “They’re extremely rare in the overall population yet present in more than half of all cases of SPTCL. Moreover, no molecular cause or genetic diagnosis has so far been determined for the disease. We therefore concluded that it was a germline mutation, occurring in parental gametes and affecting every cell in the organism, increasing the risk to bearers of having the disease,” Valera explained.
He stressed that individuals with one of the described TIM-3 mutations will not necessarily develop SPTCL and that individuals without them could develop the disease for reasons as yet unknown.
Immunology
To determine the exact effect of the mutations on T lymphocytes, the researchers used kidney tumor cells, a model widely used in studies of this type. The cells were transfected with the mutations. Unlike tumor cells without any genetic alterations, the mutant cells exhibited no expression of TIM-3 in T cells.
“When TIM-3 isn’t expressed, the functions of these defense cells can’t be controlled and the immune system becomes vulnerable,” Valera said.
Altering TIM-3 with medication to combat lymphoma is one therapeutic option. The use of antibodies to target checkpoints and activate the immune system won American immunologist James P. Allison and Japanese immunologist Tasuku Honjo the 2018 Nobel Prize in Physiology or Medicine.
Other immunosuppressants with more global anti-inflammatory action, such as cyclosporine (which inhibits proteins that suppress the immune response), have been used with positive results to treat some lymphomas, including SPTCL, as well as melanomas and brain tumors.
Now that SPTCL is known to be linked to an altered checkpoint protein, however, the researchers warn that intervening in this manner may incur risks and urge additional caution when using the strategy.
“This is the first time a human disease has been associated with a checkpoint, and we must consider whether altering the checkpoint could increase the number of immune diseases, including other kinds of cancer,” Valera said. “Therapeutic suppression of the TIM-3 checkpoint could have adverse consequences. The strategy can’t be extrapolated to all kinds of cancer.”
Immunosuppression remains the most advisable treatment for SPTCL, in which drugs such as steroids and cyclosporine are used to inhibit the activity of the immune system with the aim of countering its tendency to attack the organism instead of protecting it.
In some cases, immunosuppression alone is enough to return the organism to its normal state. In others, the disease persists, and chemotherapy is required. There are patients, however, who suffer from hemophagocytosis, in which macrophages engulf (“eat”) healthy bone marrow cells instead of destroying cancer cells. In this study, all lymphomas with mutations progressed to hemophagocytosis.
This disorder affects blood production and can lead to infection, bleeding and anemia. In these cases, when standard immunosuppression therapy fails, it is necessary to consider a bone marrow transplant to replace the immune system completely.
The article “Germline HAVCR2 mutations altering TIM-3 characterize subcutaneous panniculitis-like T cell lymphomas with hemophagocytic lymphohistiocytic syndrome” (doi: 10.1038/s41588-018-0251-4) by Tenzin Gayden et al. can be retrieved from: www.nature.com/articles/s41588-018-0251-4.
Source: https://agencia.fapesp.br/30247