

Phylogenomic analysis shows that pathogen isolated in Brazilian hospital does not belong to the genus Leishmania. Researchers are investigating whether this species alone can cause severe disease or intensifies symptoms in co-infected patients (image: Roque Pacheco Almeida)
Published on 05/12/2021
By Karina Toledo | Agência FAPESP – Brazilian researchers believe they have identified in patients treated at the University Hospital (HU) in Aracaju, state of Sergipe, a new species of parasite that can cause a disease similar to visceral leishmaniasis but is resistant to the treatments currently available. At least one person has died from complications associated with infection by the parasite.
Results of the research, supported by FAPESP, were published September 30th in the journal Emerging Infectious Diseases. Phylogenomic analysis showed that the recently discovered parasite does not belong to the genus Leishmania, which comprises over 20 species that cause different types of leishmaniasis: visceral, cutaneous and diffuse – the latter involves skin and mucosal lesions.
“From the phylogenetic standpoint, the species analyzed in this study is closer to Crithidia fasciculata, a mosquito parasite that cannot infect humans or other mammals. We managed to infect mice with it, and for this reason we believe it’s a new protozoan, which we propose to call Cridia sergipensis,” said João Santana da Silva, a professor at the University of São Paulo’s Ribeirão Preto Medical School (FMRP-USP) and a member of the Center for Research on Inflammatory Diseases (CRID), one of the Research, Innovation and Dissemination Centers (RIDCs) funded by FAPESP.
The first case was confirmed in a 64-year-old man, first treated in 2011 for classic symptoms of visceral leishmaniasis: fever, enlarged spleen and liver, and decreased production of all types of blood cells (pancytopenia).
“He was given the standard treatment and improved, but suffered a relapse only four months later. He was then treated with the best drug available for these cases – liposomal amphotericin B – and responded, but suffered another relapse eight months later. This time he developed papular rash all over his body, which isn’t usual in visceral leishmaniasis,” said Roque Pacheco Almeida, a professor at the Federal University of Sergipe (UFS), head of the University Hospital’s Molecular Biology Laboratory and a researcher affiliated with CRID.
“Unfortunately the patient died after the relapses, spread of the disease to his skin and an operation to remove his spleen, as recommended in severe cases that don’t respond to treatment.”
A biopsy of the skin lesions found defense cells full of parasites, which were isolated and cryopreserved for analysis. The researchers also isolated samples of bone marrow during the relapses, and samples of the spleen after its surgical removal.
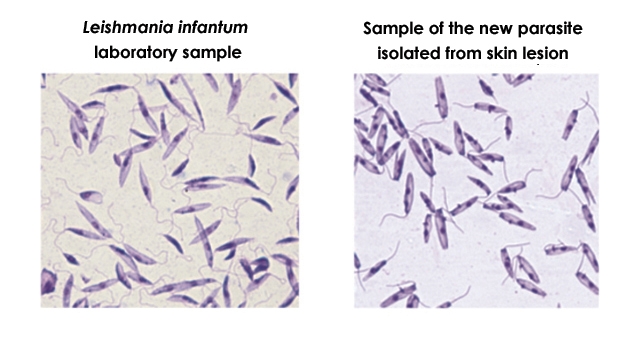
Initially the group thought the patient had been infected atypically by Leishmania infantum. However, the molecular tests available for diagnosis of this pathogen were all inconclusive in the analyses performed on the parasites isolated from bone marrow and skin lesions.
Mice infected with the sample isolated from the patient’s skin developed skin lesions and mild liver damage. Surprisingly, the experimental infection with the new parasite was more aggressive in the skin than in the animals used as positive controls (infected with Leishmania major, the species that causes cutaneous leishmaniasis). The animals infected with the bone marrow parasite displayed typical symptoms of visceral leishmaniasis, such as infected liver and spleen, but no skin alterations.
“We realized the patient could be infected with two different parasites – hence the severity of his condition,” Almeida said.
Whole genome
The researchers decided to perform a whole-genome analysis of the parasites isolated from the patient in order to find out exactly what they were dealing with.
“We also had samples of other species of Leishmania sequenced. They included L. amazonenses, L. braziliensis, and L. infantum, all of which we had in our lab,” Silva said. The aim was to see if there were any similarities.
The bioinformatics analysis that revealed the phylogenetic similarity between the new species and C. fasciculata was conducted in the United States by José Marcos Ribeiro at the National Institute of Allergy & Infectious Diseases (NIAID) and Sandra Regina Costa Maruyama, a researcher in the Department of Genetics and Evolution at the Federal University of São Carlos (UFSCar) with support from FAPESP’s Young Investigator Grants (YIG) program.
“We compared the genomes of the parasites isolated from the patient’s skin and bone marrow, and concluded that they were the same species and that this species can infect both internal organs and skin,” Maruyama said. “We also performed a whole-genome analysis of parasites isolated from two other patients in Aracaju who weren’t responding to treatment, confirming that they too belonged to the new species. Another 150 isolates are awaiting whole-genome sequencing and analysis.”
According to Maruyama, preliminary results – obtained from an analysis of fragments of the genome identified as key to characterization of the species – suggest that most of the protozoans present in the 150 isolates match the profile of Cridia sergipensis.
“We used bioinformatics tools to identify regions of the genome that are specific to this species, and validate them experimentally. Based on these findings we were able to develop a molecular test to diagnose the new parasite. In parallel we also had to develop a specific molecular test for Leishmania infantum. Now we can identify the parasite that has infected patients and also detect any co-infections,” Maruyama told Agência FAPESP.
The next step, she added, is to make the methodology even more sensitive so that the molecular test can be performed directly with blood samples from patients with suspected leishmaniasis.
Unanswered questions
The research priorities noted by the authors of the article include a search for drugs that can kill the new parasite efficiently. According to Almeida, testing of various compounds is already under way.
Another challenge is discovering how the pathogen emerged and how it is transmitted to humans. “It could be the result of crossing between Leishmania and another genus, or of a genetic mutation that has given Crithidia the capacity to infect mammals. Or it may always have existed in the wild and come closer to humans as they occupied its space,” Almeida said.
For Maruyama, a top priority is finding out whether Cridia sergipensis alone is capable of causing severe and potentially fatal disease or whether the cases observed resulted from double infection. “It could be that the new parasite is helping to exacerbate typical cases of visceral leishmaniasis,” she said.
According to Almeida, this would explain why the visceral leishmaniasis lethality rate in the state of Sergipe was 15% in 2016, compared with a predicted rate of only 6%. Suspected cases were treated by medical teams in the Infectology and Pediatrics Departments of Sergipe University Hospital, linked to Empresa Brasileira de Serviços Hospitalares (EBSERH), a state-owned hospital management company.
The article Non-Leishmania parasite in fatal visceral leishmaniasis-like disease, Brazil can be read at wwwnc.cdc.gov/eid/article/25/11/18-1548_article.
Source: https://agencia.fapesp.br/31581