

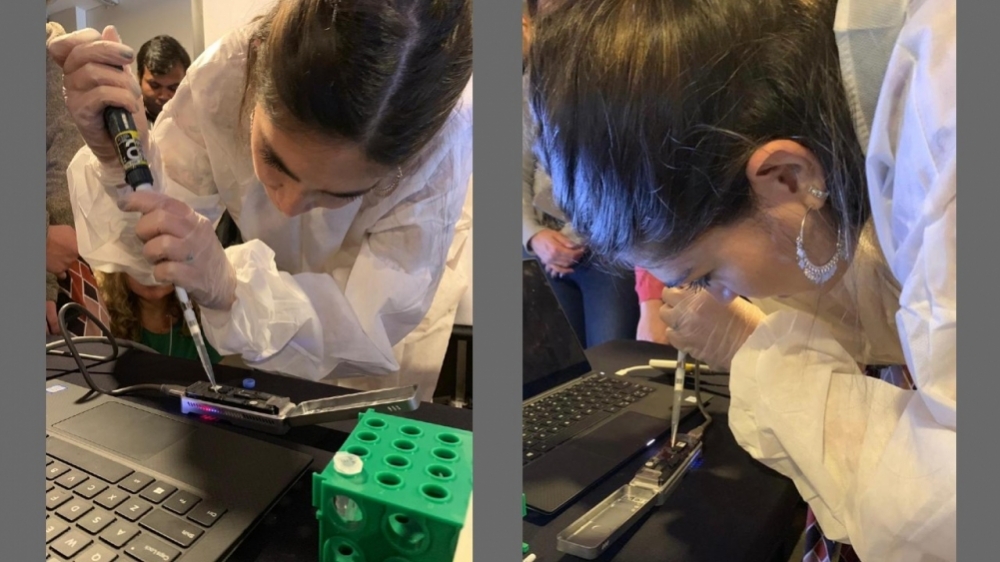
A protocol developed by the Brazil-UK Center for Arbovirus Discovery, Diagnosis, Genomics and Epidemiology (CADDE) was used to analyze a sample from the first Brazilian patient with a confirmed diagnosis. The technology can also be used to detect unknown emerging viruses (photo: CADDE)
Published on 06/20/2022
By Karina Toledo | Agência FAPESP – Researchers at the Brazil-UK Center for Arbovirus Discovery, Diagnosis, Genomics and Epidemiology (CADDE) have completely sequenced the genome of the monkeypox virus (MPXV) in only 18 hours, using a sample isolated from the first patient with a confirmed diagnosis of the disease in Brazil.
They were able to achieve the feat by adapting to MPXV a metagenomics technique developed during the PhD research of Ingra Morales Claro, who was supported by a scholarship from FAPESP. The principal investigator was Ester Sabino, a professor at the University of São Paulo (USP) in Brazil. Sabino also led the first sequencing of SARS-CoV-2 in Brazil in March 2020, and genomic analysis of the first cases of infection by the gamma variant in Manaus about a year later (more at: agencia.fapesp.br/32656 and agencia.fapesp.br/35414).
The CADDE team posted the results on June 9 to virological.org, where virologists from around the world share information on pathogens of interest in real time.
“We received the sample from a patient undergoing treatment at Emílio Ribas Hospital at 4:00 p.m. on Tuesday [June 7], and at 10:00 a.m. the next morning the genome of the virus, which has almost 200,000 base pairs [many more than SARS-CoV-2, which has 30,000], was sequenced and analyzed. The methodology we’ve developed is 45% faster on average than conventional metagenomics techniques. It’s also cheaper, costing about USD 30 per sample,” Claro told Agência FAPESP.
As Sabino explained, scientists typically opt for metagenomics when they need to identify a novel emerging virus (as SARS-CoV-2 was in 2019) or detect a known virus in patient samples when the specific reagents they need are not to hand (as with MPXV now).
This is because the RT-PCR test, the gold standard for diagnosing COVID-19 and several other diseases, requires primers – short nucleic acid sequences that provide a starting point for DNA synthesis and complement the viral sequences that begin replication of the genetic material. In addition, the result has to be compared with negative and positive controls.
“In the initial stage of an epidemic involving a novel infectious agent, one of the main bottlenecks holding up diagnosis of cases is a lack of specific primers and positive controls. This technique of ours can be useful in such situations. It can identify unknown pathogens for which there are no reagents,” Sabino said.
The sooner the index (first) case is detected, the greater the probability that an emerging virus can be contained, Claro added.
The primers used in metagenomics are random (not specific to a given virus or bacterium), enabling all the genetic material in a biological sample to be sequenced, including that of the host (human in this case) as well as any other pathogens inhabiting the host. The resulting data is analyzed using bioinformatics and compared with a reference panel.
“This was exactly what we did with MPXV. We mapped the data against a sequence of the virus already available for research purposes and were able to prove that it was indeed monkeypox,” Claro said.
Faster sequencing
The first Brazilian case of monkeypox was officially confirmed on June 9 by Adolfo Lutz Institute (IAL), São Paulo state’s reference laboratory for epidemiological surveillance. IAL conducted the metagenomics analysis on a platform known as Illumina, one of the technologies that have been used to detect MPXV in Europe and the United States, and considered the gold standard for this purpose. Sequencing by this method takes 48 hours on average.
The group used MinION, a portable sequencer developed by Oxford Nanopore Technologies, adapting the protocol used to sequence zika virus since 2015 and SARS-CoV-2 since 2020 to make it faster.
“One of the advantages of this new protocol is that it shortens the time taken to prepare the sample for sequencing, which is 5 hours and 40 minutes instead of 14 hours,” Claro said.
The error rate is slightly higher than for Illumina, so the CADDE team set out to perform 300 redundant reads for every region of the viral genome. “When we cover the same region several times and get the same result, we can be sure no readout errors are involved,” she explained.
The next step was to assemble the phylogenetic tree for the MPXV isolated in Brazil. To this end, the CADDE team compared the sequence obtained at USP with 102 others published this year by scientists in Belgium, Germany, Portugal, Spain, the United Kingdom and the United States. The aim was to measure the degree of similarity between the sequences and thereby obtain clues to their evolutionary relationship.
“We downloaded all the whole-genome sequences produced in 2022 [until June 9], aligned them, and plotted the phylogenetic tree,” Claro said. “We found that the MPXV detected here slots into the same major clade [group that evolved from a common ancestor] as the viruses sequenced in Europe and the US. When we compared the reference genome updated by the CDC [the US public health surveillance authority], we detected only three mutations.”
The first MPXV genome sequenced in 2022 had 47 mutations compared with the last case described before that (in 2018, in Africa).
“Other research groups are studying what these mutations represent and whether they contributed to the rise in case numbers. Here at CADDE, we’ll continue to analyze forthcoming cases. We plan to continue sequencing the virus in order to monitor its evolution,” Claro said.
Although MPXV is known for causing monkeypox, it mainly infects rodents in Africa. It belongs to the Orthopoxvirus genus, as does human smallpox, eradicated in 1980.
The initial symptoms of monkeypox in humans are fever, headache and muscle pain. These are not very specific and closely resemble the symptoms of flu. A few days after the onset of fever, however, skin lesions with a high viral load appear. The disease spreads by direct contact with the lesions or with garments, bedclothes or towels used by someone who has them. It may also be transmitted by coughing or sneezing.
Until the start of this year, the disease was common only in Central Africa, but new cases have been detected in 33 countries, most of which have no prior record of monkeypox in humans.
Source: https://agencia.fapesp.br/38928