

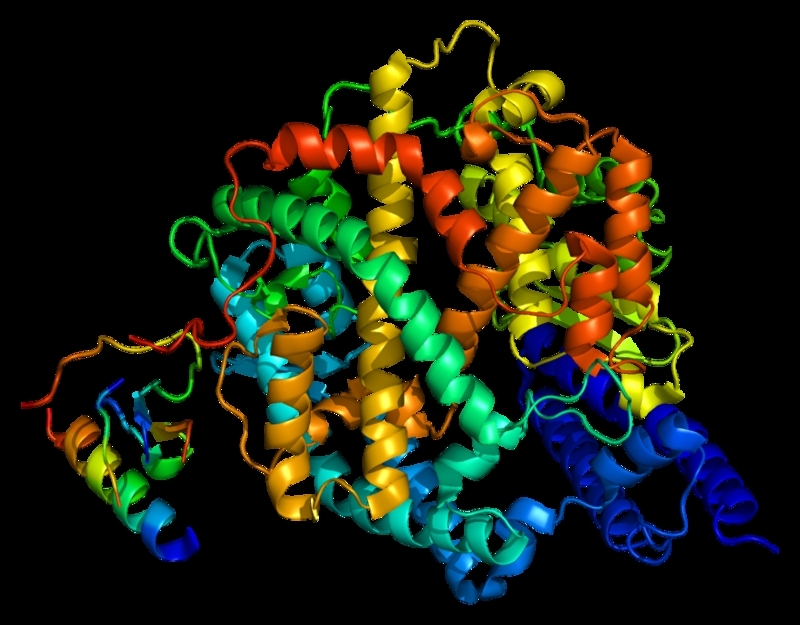
The gene ACE-2 expresses the messenger RNA that regulates production of angiotensin-converting enzyme 2, used by the novel coronavirus to infect lung cells (image: Wikimedia Commons)
Published on 03/25/2021
By Karina Toledo | Agência FAPESP – A study conducted at the University of São Paulo (USP) in Brazil can help understand why the mortality rate from COVID-19 is higher among people with chronic health problems such as high blood pressure, diabetes, or chronic obstructive pulmonary disease (COPD).
According to an article on the study published on MedRxiv.org, alterations in the patient’s metabolism caused by these diseases can trigger a series of biochemical events that lead to increased expression of the gene ACE-2, which encodes a protein to which the virus binds in order to infect lung cells.
“Our hypothesis is that owing to increased expression of ACE-2 and other genes that facilitate infection by SARS-CoV-2, such as TMPRSS2 and FURIN, these patients have more infected cells and are therefore more severely stricken by the disease. However, this hypothesis must be confirmed by experimental studies,” Helder Nakaya, a professor in the School of Pharmaceutical Sciences (FCF-USP) and principal investigator for the project supported by FAPESP, told Agência FAPESP.
He said the findings can help identify molecular targets for future drug development.
According to Nakaya, the gene ACE-2 expresses the messenger RNA that regulates production of angiotensin-converting enzyme 2, which acts as a vasodilator and is part of the renin-angiotensin-aldosterone system, a hormone system that governs blood pressure.
“After the 2003 outbreak of SARS [severe acute respiratory syndrome], scientists discovered the key role played by the gene ACE-2 in enabling the virus [SARS-CoV-2] to enter human cells. The same applies to the novel coronavirus. For this reason we decided to investigate whether expression of this gene is altered in patients with chronic diseases,” said Nakaya, who is also affiliated with the Center for Research on Inflammatory Diseases (CRID), a Research, Innovation and Dissemination Center (RIDC) funded by FAPESP and hosted by the University of São Paulo’s Ribeirão Preto Medical School (FMRP-USP).
Bioinformatics
The first step in the investigation was a search of Medline, a bibliographic database of life sciences and biomedical information from almost 5,000 journals published in more than 70 countries, maintained by the US National Library of Medicine (NLM), to scan for scientific articles on the diseases of interest to the group, including COPD, hypertension, diabetes, cardiovascular disorders, lung cancer, chronic renal insufficiency, autoimmune diseases, pulmonary fibrosis, asthma, and pulmonary hypertension.
“We identified 8,700 articles. It wouldn’t have been feasible to read all of them, so we used a text mining tool to screen out everything except articles containing information on the genes involved in these diseases. The set of genes at which we arrived included ACE-2,” Nakaya explained.
The researchers then re-analyzed data relating to the transcriptome (all RNA molecules expressed by the human genome) of over 700 lung samples available in public repositories such as the Gene Expression Omnibus (GEO).
“This is free-to-access data collected in previous studies,” Nakaya said. “We compared the gene expression profiles of patients with chronic diseases that affect the lungs with those of healthy people, who served as controls. We also compared the profiles of smokers and non-smokers. The focus was on the lungs of people who were not infected by the novel coronavirus but had diseases that made them susceptible to severe manifestations of COVID-19. We wanted to understand the differences.”
The meta-analysis showed expression of ACE-2 to be significantly increased in the diseases, Nakaya said.
The next step was to find out which other genes had expression profiles that were similar to that of ACE-2 or the reverse. “This kind of correlation analysis helps orient hypotheses, although it doesn’t establish causality. Instead of looking at 500 genes, we can concentrate on eight genes with expression profiles that correlate with the gene of interest, and in future do experiments to see what happens when they are inhibited or stimulated,” Nakaya said.
The group then realized that the expression profiles of samples with increased expression of ACE-2 also displayed certain enzymes capable of modifying the functioning of histones, a type of protein found in cell nuclei that binds to DNA and helps control the activity of genes. In scientific jargon this phenomenon is known as epigenetic modification (when gene expression patterns change without any change in DNA).
“Our findings suggest these chronic diseases change the organism’s epigenetic program. We don’t know exactly how, but it seems they make these enzymes more active and thereby increase expression of ACE-2, favoring infection of lung cells by SARS-CoV-2,” Nakaya said.
The discovery could lead to the development of compounds that inhibit the activity of some of these histone-modifying enzymes and modulate expression of ACE-2 to protect the lungs, he added.
The article “ACE2 expression is Increased in the lungs of patients with comorbidities associated with severe COVID-19” can be read in preprint (not yet peer reviewed) at: www.medrxiv.org/content/10.1101/2020.03.21.20040261v1.
Source: https://agencia.fapesp.br/32947