

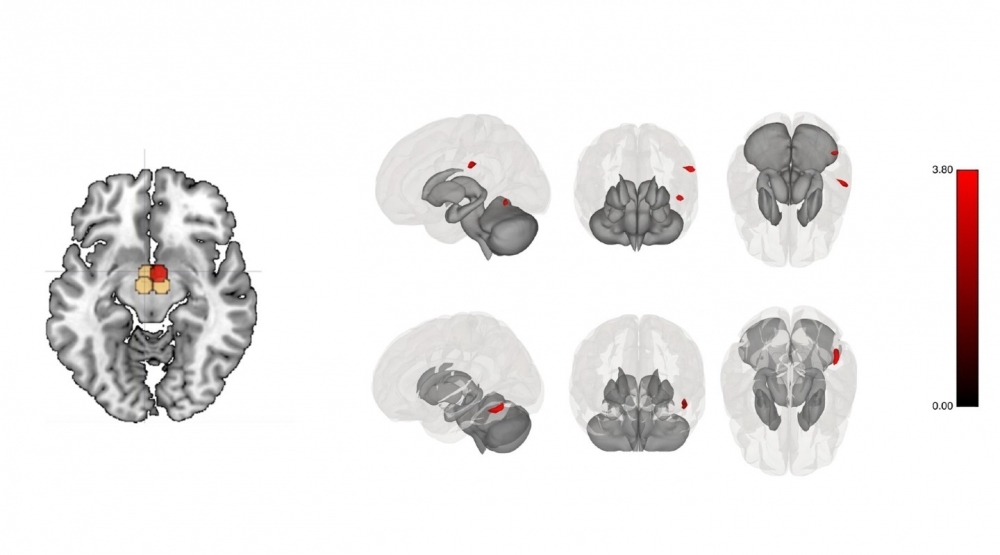
Hypothalamic connectivity: red indicates increase in brain connectivity after intervention, black indicates decrease, beige indicates no change. Panel on left shows areas investigated, with right medial hypothalamus highlighted in red because it changed after post-bariatric exercise. Panel on right shows increased connectivity between sensory and visual areas and right medial hypothalamus, including supramarginal gyrus and temporal regions (image: researchers’ archive)
Published on 03/20/2023
By Luciana Constantino | Agência FAPESP – Physical exercise practiced by patients submitted to bariatric surgery acts on brain regions involved in food intake, reducing hunger or accelerating satiety, for example. This was the result observed in a clinical trial conducted at Hospital das Clínicas (HC), the hospital complex run by the University of São Paulo’s Medical School (FM-USP) in Brazil. An article on the study, pointing to positive effects of exercise on obesity-related conditions in post-bariatric patients, is published in the International Journal of Obesity.
The study showed that an exercise training program starting three months after bariatric surgery produced functional alterations in brain networks associated with food intake and modified by obesity. The findings confirm the hypothesis that exercise and bariatric surgery act synergistically on the connectivity among brain regions associated with cognition, reward and emotional regulation, potentially moderating hunger and enhancing satiety.
According to the article, exercise increased the connectivity between the hypothalamus (the brain region that controls homeostasis, including regulation of appetite and energy expenditure) and the brain’s sensory areas. At the same time, it apparently decreased the link between the default mode network, which is more active during a resting state, and the salience network, the brain region involved in decision-making.
The researchers also found that exercise after bariatric surgery appeared to modulate the medial hypothalamic nucleus involved in appetite suppression and increased energy expenditure.
“The regulation of energy expenditure is governed by multiple internal and external signals. People with obesity display major dysregulation of brain regions associated with appetite and satiety. Our study showed that exercise by post-bariatric patients helped ‘normalize’ these complex networks so as to improve the central control of food intake. For example, some of these regions are activated and connect more intensely in people with obesity when they eat fatty or sugary food, increasing their desire to consume such food. We found that exercise counteracts this effect, at least in part,” Bruno Gualano, last author of the article, told Agência FAPESP. Gualano is a professor at FM-USP.
The study was supported by FAPESP via a research grant for the project “Effects of exercise training in patients undergoing bariatric surgery: a randomized clinical trial” and was part of the PhD research of Carlos Merege Filho, first author of the article, with a scholarship from FAPESP. The co-authors included Hamilton Roschel, Marco Aurélio Santo, Sônia Brucki, Claudia da Costa Leite, Maria Concepción García Otaduy and Mariana Nucci (all of whom are affiliated with HC-FM-USP); and John Kirwan of Pennington Biomedical Center (USA).
Considered one of the world’s main public health problems, obesity is a chronic disease characterized by excessive body fat accumulation and a major risk factor for cardiovascular and musculoskeletal disorders, as well as severe COVID-19. The parameter used for diagnosis in adults is body mass index (BMI), defined as weight in kilograms divided by height squared in meters. A BMI between 25 and 29.9 indicates overweight, while 30 or more signals obesity, according to the World Health Organization (WHO).
Brazil has one of the highest rates of overweight and obesity in the world. According to projections, almost 30% of the adult population will be obese in 2030. A billion people, or 17.5% of the world’s adult population, will be obese by then, according to the World Obesity Atlas 2022 published by the World Obesity Federation.
Importance
From the clinical standpoint, Gualano believes, the findings suggest that exercise should be considered an important complementary therapy to improve brain functions and enhance the known benefits of bariatric surgery, such as a reduction in cardiometabolic risk factors, as well as preservation of muscle mass and bone health.
He and his group have been conducting research in this field since 2018, as evidenced by other publications, one of which showed that exercise attenuated and reversed loss of muscle mass, improving muscle strength and function in post-bariatric patients. Genotypic and phenotypic analysis evidenced metabolic and structural remodeling of skeletal muscle.
In another study, exercise reduced risk factors for diseases associated with obesity, such as diabetes, high blood pressure and atherosclerosis (hardening of the arteries), by increasing sensitivity to insulin, combating inflammation and improving the health of blood vessels.
Methods
The randomized clinical trial reported in the International Journal of Obesity involved 30 women aged between 18 and 60 who had been submitted at HC-FM-USP’s bariatric surgery unit to a Roux-en-Y gastric bypass, which creates a small stomach pouch to restrict food intake and bypasses a large portion of the small intestine to limit calorie absorption. A majority of patients admitted to the unit are women.
Half the study sample were randomly assigned to a six-month exercise program of resistance and aerobic training three times a week, starting three months after the operation and supervised by a team of physical education professionals.
Clinical, laboratory and brain functional connectivity parameters were assessed at the start of the trial, as a baseline, and again three and nine months after the operation. Functional magnetic resonance imaging (fMRI) was used to detect connectivity between anatomically distinct brain areas organized as networks, and to analyze the combined effects of the surgical procedure and exercise training. Data collection began in June 2018 and ended in August 2021.
“The literature has already shown that post-bariatric patients have many brain alterations compatible with improved control of appetite, satiety and hunger in neural circuits that govern food intake. Our study found that exercise training bolstered this response,” Gualano said, noting the importance of lifestyle changes to maintain the benefits of weight loss for people with obesity.
Bariatric surgery can currently be performed on patients with a BMI of between 30 and 35 and type 2 diabetes that has not been controlled for more than two years, and patients with a BMI over 35 who have other diseases associated with overweight, such as high blood pressure, sleep apnea or hepatic steatosis (fatty liver disease). For people with comorbidities, the recommended BMI is over 40.
In the past five years, 311,850 bariatric surgeries have been performed in Brazil; 14.1% were paid for by the SUS (Sistema Único de Saúde), the national health service. The rest were covered by insurance policies or paid for privately, according to the Brazilian Bariatric and Metabolic Surgery Society (SBCBM).
“Regular exercise is known to induce several physiological adaptations that translate into health benefits. These benefits are reversed if the patient stops exercising regularly. Our study didn’t measure the duration of the brain changes induced by exercise, however. They’re highly likely to diminish and possibly even go into reverse as the amount and intensity of exercise decrease. It’s crucial to adopt a healthy lifestyle in order for the responses to bariatric surgery to be long-lasting,” Gualano said.
Next steps for the research group will include studying the effects in people with obesity of exercise and diet combined with other weight loss strategies, including new drugs such as peptide analogs or incretin mimetics, a class of medications commonly used to treat type 2 diabetes. Incretins are gut hormones that aid digestion and blood sugar control by signaling to the brain to stop eating after a meal.
In early January, the National Health Surveillance Agency (ANVISA) approved semaglutide as an anti-obesity drug for long-term weight management. The drug had previously been approved only for patients with type 2 diabetes. It is the first injectable anti-obesity medication available in Brazil and is supposed to be administered once a week. It is said to enhance satiety, modulate appetite and control blood sugar.
The article “Exercise modifies hypothalamic connectivity and brain functional networks in women after bariatric surgery: a randomized clinical trial” is at: www.nature.com/articles/s41366-022-01251-8.
Source: https://agencia.fapesp.br/40943