

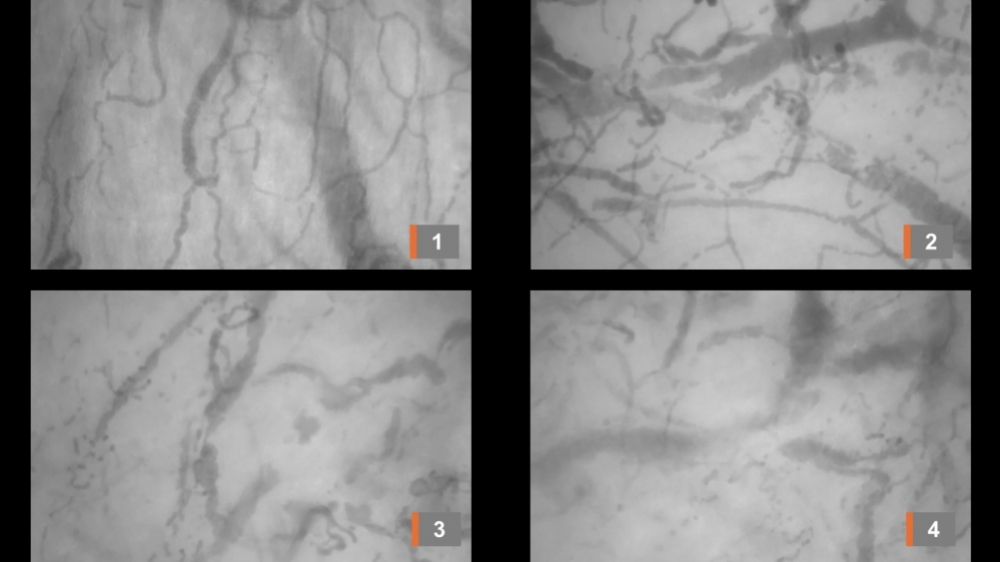
A study involving 13 patients requiring intubation for mechanical ventilation reinforces the theory that coagulation disorders resulting from an exacerbated inflammatory response to SARS-CoV-2 may explain some of the most severe symptoms of the disease (image 1 shows normal microcirculation; images 2 and 3 show signs of circulatory problems; image 4 captures acute thromboembolic obstruction. Credit: Carlos Henrique Miranda)
Published on 03/19/2021
By Karina Toledo | Agência FAPESP – Researchers at the University of São Paulo’s Ribeirão Preto Medical School (FMRP-USP) in Brazil have filmed clotting in small blood vessels under the tongues of patients hospitalized with severe COVID-19. A paper reporting this in vivo demonstration of sublingual microvascular thrombosis is published on medRxiv. The findings reinforce the theory that blood clotting disorders resulting from an exacerbated inflammatory response to SARS-CoV-2 may explain some of the most severe symptoms of COVID-19, including respiratory failure and pulmonary fibrosis.
Evidence to support the theory emerged in April when researchers at the university’s São Paulo Medical School (FM-USP) found mini-clots (microthrombi) in the small blood vessels that irrigate the lungs during autopsies of people who died of COVID-19 (read more at: agencia.fapesp.br/32955/).
“There was still a measure of doubt whether these clotting disorders were due to long stays in hospital ICUs [intensive care units] or to the inflammatory response triggered by the virus. We observed the formation of microthrombi on the first day in the hospital,” Carlos Henrique Miranda, a professor in FMRP-USP’s Department of Internal Medicine, told Agência FAPESP.
The article, available as a preprint (not yet peer-reviewed), describes the researchers’ analysis of sublingual microcirculation in 13 patients with severe COVID-19 requiring intubation for mechanical ventilation. The images were obtained on the day after admission to the hospital with a handheld video capillary microscope placed under the tongue with a polarized light source to illuminate the tissue, showing live movement of red blood cells as they traveled through microvessels. The study was supported by FAPESP.
“We originally set out to use the microscope to study clotting disorders in patients with sepsis [systemic inflammation typically triggered by a localized bacterial infection] but had to put this project on hold because of the pandemic,” Miranda said. “It also proved difficult to import the equipment. We succeeded thanks to assistance from FAPESP’s import division and decided to focus instead on COVID-19 patients.”
The sublingual mucosa was chosen because it is easily accessible in a noninvasive manner. “In these microvessels, we observed multiple filling defects, indicating the absence of red blood cells,” Miranda said. “We inferred that this was due to obstruction of the blood flow by clotting. In some patients, we were able to watch the vessels thrombosing right before our eyes.”
According to Miranda, the coagulation disorder caused by SARS-CoV-2 appears to be “predominantly thrombotic in nature” and “very intense”, unlike what is seen in bacterial sepsis.
The problem is associated with interleukins, proteins that stimulate immune responses including inflammation. In the case of COVID-19, an interleukin storm activates a clotting cascade in which platelets clump together to form thrombi, blocking small vessels in the lungs and causing microinfarcts; tiny tissue lesions and cell death due to insufficient blood flow gives rise to connective tissue in a process of fibrotic scarring. In addition, microthrombi where blood vessels meet the alveoli in the lungs prevent oxygen from reaching smaller arteries, thus impairing oxygenation of the blood (read more at agencia.fapesp.br/33233).
“These inflammatory factors that lead to the formation of microthrombi are systemic and therefore don’t only affect the lungs. Several other organs may be damaged. We were able to record the effects in the sublingual region,” said Miranda, who is currently leading a clinical study designed to evaluate the use of heparin, one of the most widely used anti-coagulant drugs worldwide, to improve blood oxygen saturation in patients with respiratory failure caused by the novel coronavirus.
“We planned to use the capillaroscope to analyze the effects of this treatment on sublingual microcirculation, but the epidemic surged here in Ribeirão Preto, and the priority is now to care for COVID-19 patients,” Miranda said.
The article “In vivo demonstration of microvascular thrombosis in severe COVID-19” can be retrieved from www.medrxiv.org/content/10.1101/2020.07.09.20149971v1.
Source: https://agencia.fapesp.br/33909