

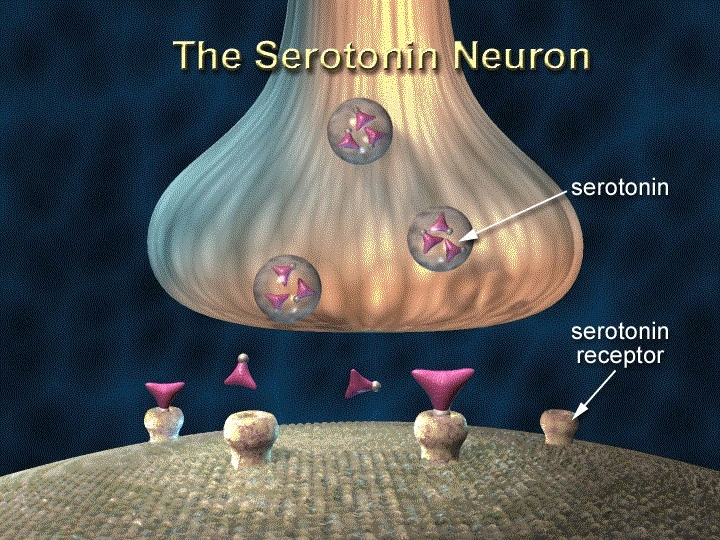
An experiment in rats performed in Brazil shows that this “wellbeing hormone” helps modulate the immune system, induces anti-inflammatory effects, and prevents complications such as a sharp drop in body temperature and blood pressure (image: NIDA / NIH)
Published on 05/04/2021
By Maria Fernanda Ziegler | Agência FAPESP – Known as the “wellbeing hormone” in recognition of its key role in mood regulation, serotonin also modulates severe systemic inflammation, such as that which occurs during sepsis. An article published in Brain, Behavior, and Immunity describes this neurotransmitter for the first time as a possible mediator of neuroimmune interactions that can attenuate inflammation not only in the central nervous system but also throughout the organism.
The study was conducted in Brazil by researchers affiliated with the University of São Paulo’s Ribeirão Preto School of Dentistry (FORP-USP), Nursing School (EERP-USP) and Medical School (FMRP-USP). The injection of serotonin into the central nervous system of rats had anti-inflammatory effects, lowering levels of immune system signaling molecules (proinflammatory cytokines) in the blood plasma and spleen. The injected serotonin also prevented hypothermia and hypotension (low blood pressure). The study was part of a Thematic Project supported by FAPESP.
“Serotonin’s capacity to inhibit systemic inflammation was unknown until now. We reached this conclusion in two studies, one published in 2017 on mild systemic inflammation such as that which occurs during the flu or a urinary infection, and now in this investigation involving severe systemic inflammation, which surprised us even more because we observed such a positive effect in a much more severe condition corresponding to sepsis,” said Luiz Guilherme Branco, Full Professor at FORP-USP and coauthor of the article.
Lethal disease
Sepsis derives from a dysregulated inflammatory response of the organism in the presence of an infectious agent. The defense system combats the pathogen in an exaggerated manner. Other signs of sepsis include a high or low body temperature, low blood pressure and impaired blood flow, leading to multiple organ failure.
Organ failure and an abrupt drop in blood pressure are the two main factors in septic shock, which is a fatal condition for many patients. In Brazil, 55.7% of sepsis cases in ICUs end in death (read more at: agencia.fapesp.br/26862).
To investigate the role of serotonin in neuroimmune interactions, the researchers performed two types of experiments. In the first, which involved mild systemic infection models, the substance was injected into the central nervous system of rats. Half an hour after the intracranial injection, the rats received a small dose (100 µg/kg) of lipopolysaccharide, a toxin present in the cell walls of some bacteria.
Comparing the rats given serotonin and a control group given only the toxin, the researchers found that the neurotransmitter had an anti-inflammatory effect on the brain and periphery and lowered the fever caused by mild systemic inflammation.
In an article published this year, the researchers describe the same experiment but with a fifteen-fold dose of the toxin (1.5 mg/kg), leading to sepsis-like severe systemic inflammation. In this experiment, serotonin not only lowered the level of pro-inflammatory cytokines but also prevented hypothermia and hypotension.
“We believe the effects of serotonin are due to activation of an anti-inflammatory reflex during systemic inflammation, whereby neuronal activity modulates immunity and reduces the levels of inflammatory cytokines via neural connections from the brain to other organs, especially the spleen,” said Clarissa Mota, a researcher at FMRP-USP with a doctoral scholarship from FAPESP and first author of the article.
According to Mota, the next steps in this research line will consist of investigating in greater depth the mechanisms involved in the brain regions that produce serotonin or combat systemic inflammation.
“The discovery that serotonin also plays a role in the modulation of inflammation paves the way to studies on the development of new therapies against sepsis and other inflammatory disorders,” she said. “We’re assembling the pieces of a jigsaw puzzle to glean a better understanding of the physiopathology of inflammation and of the therapeutic functions of serotonin. Decades ago, [body] systems were studied separately. Today, we know the organism is like a connected network with all systems working hand in hand.”
As a product of tryptophan metabolism, serotonin is part of this network and performs a number of functions in the brain and other organs. The neurotransmitter acts as a messenger in synapses (the links between neurons) and modulates communication – hence, its involvement in the regulation of physiological processes such as sleep, breathing, mood, platelet coagulation and digestion, as well as modulation of the immune system, as the researchers have now shown.
Mota explained that because this was an initial study to investigate the role of serotonin in the neural mechanisms of inflammation and in therapy, it was decided to perform a pretreatment test.
“Experimentally speaking, we began by investigating the effects of pretreatment to find out more about serotonin’s role in modulating inflammation. Since our research has shown that serotonin can prevent many of the effects of systemic inflammation, our next steps will focus on the search for curative treatment instead of [preventive] pretreatment and on a deeper understanding of how serotonin can modulate inflammation,” Mota said.
Antidepressants and anxiolytics
The translational potential of the study is highlighted in an editorial by Christoph Rummel, a researcher at the University of Giessen in Germany who has contributed to the understanding of the mechanisms that mediate neuroimmune communication pathways during inflammation. “Potential translational implications for the use of serotonin reuptake inhibitors [present in medications] to treat major depressive disorders as well as chronic peripheral inflammation represent exciting new avenues, which need to be further investigated,” Rummel writes in the editorial.
According to Brazilian researchers, by injecting serotonin into the rats’ central nervous system, their experiment mimicked the action of antidepressant and anxiolytic medications that enhance the availability of this neurotransmitter in the patient’s brain.
“Serotonin reuptake inhibitors have been used by the pharmaceutical industry to treat psychiatric disorders such as anxiety and depression,” Branco said. “These medications increase the bioavailability of serotonin in central nervous system synaptic clefts. In this study, we observed a decrease in [endogenous] serotonin production by the organism during systemic inflammation. Administration of exogenous serotonin reversed some of the symptoms of systemic inflammation.”
The article “Central serotonin prevents hypotension and hypothermia and reduces plasma and spleen cytokine levels during systemic inflammation” (doi: 10.1016/j.bbi.2019.03.017) by Clarissa M.D. Mota, Gabriela S. Borges, Mateus R. Amorim, Ruither O.G. Carolino, Marcelo E. Batalhão, Janete A. Anselmo-Franci, Evelin C. Carnio and Luiz G.S. Branco can be retrieved from: www.sciencedirect.com/science/article/pii/S0889159118307700?via%3Dihub.
The article “Central serotonin attenuates LPS-induced systemic inflammation” (doi: 10.1016/j.bbi.2017.07.010) by Clarissa M.D. Mota, Caroline Rodrigues-Santos, Rodrigo A.R. Fernández, Ruither O.G. Carolino, José Antunes-Rodrigues, Janete A. Anselmo-Franci and Luiz G.S. Branco can be retrieved from: www.sciencedirect.com/science/article/pii/S0889159117302179?via%3Dihub.
Source: https://agencia.fapesp.br/31958