

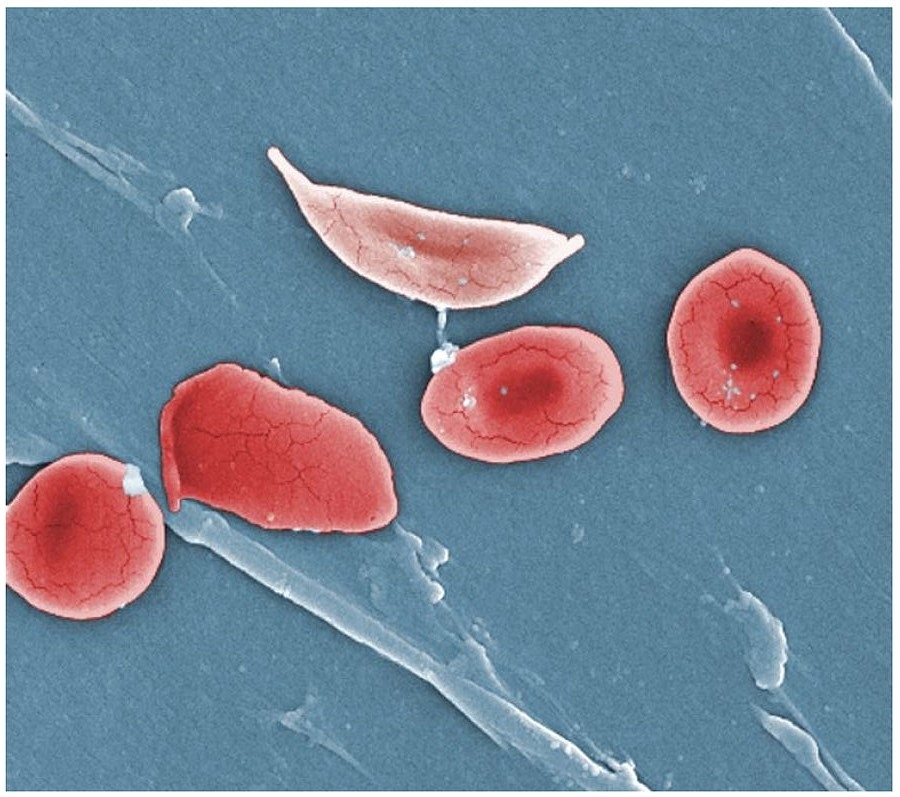
Article signed by researchers affiliated with institutions in the US, UK, Ghana and Brazil highlights recent progress in diagnosis and treatment but warns that more screening of newborns is needed (image: Anatomy & Physiology / Wikimedia Commons)
Published on 05/12/2021
By André Julião | Agência FAPESP – The promise of new treatments for sickle cell disease, a group of inherited red blood cell disorders, has never been so great, but it will only be realized if there is constant investment in health policies such as programs for screening newborns, especially in sub-Saharan Africa, where most cases occur.
This point is made in a comprehensive review of the main research findings regarding sickle disease published in Nature Reviews Disease Primers and signed by experts affiliated with institutions in the United States, United Kingdom, Ghana and Brazil.
Sickle cell disease is caused by a mutation in the gene that helps make hemoglobin, the oxygen transport protein in red blood cells. Red blood cells containing normal hemoglobin are disc-shaped, but cells with this mutation are sickle-shaped. Sickle cell anemia is the most severe disorder in the group of related diseases. Another medically important hemoglobin-related disorder is thalassemia, a hereditary form of chronic anemia with different degrees of severity.
“Major progress has been achieved in diagnosis and treatment in recent years, and there will be more, but the number of people with sickle cell disease is growing in poor countries. It’s important above all to focus on Africa and Asia, as well as Brazil, where funding of the public health system is not just not increasing but appears to be falling, so that all this progress is endangered in Brazil,” said Fernando Ferreira Costa, a full professor and researcher at the Hematology and Hemotherapy Center (Blood Center) of the University of Campinas (UNICAMP) in São Paulo State, Brazil.
Costa, the only Brazilian among the authors of the study, was referring to the existence of publicly funded blood centers and support from SUS, the national health service, for PNTN, a nationwide neonatal screening program, which administers, among other diagnostic modalities, the heel prick test, which is designed to detect hemoglobinopathies and six other diseases in newborns. Costa also stressed the importance of the free supply by the SUS of hydroxycarbamide (also known as hydroxyurea), the main drug used to treat sickle cell anemia, and the blood transfusions required by many patients.
“A lot of progress has been made in Brazil, which has successfully established centers of excellence. Diagnosis, treatment and research have all developed significantly in recent decades,” he told Agência FAPESP.
Costa is the principal investigator for the Thematic Project “Red blood cell disorders: pathophysiology and new therapeutic approaches” funded by FAPESP.
The Nature Reviews article highlights a decision by the US Food and Drug Administration (FDA) to rate the development of new treatments for sickle cell disease (SCD) as a top priority, facilitating investment by the pharmaceutical industry. As a result, many drugs targeting one or more of the mechanisms that contribute to SCD are currently being tested in humans.
“The prospects for new treatments for SCD have never looked better,” the authors conclude.
Hereditary mutation
Sickle cell anemia is the most severe and prevalent form of SCD. Sickle-shaped red blood cells are deformed and become rigid, with a tendency to polymerize – form groups that stick to the inner lining of blood vessels (endothelium) – impairing or even blocking the flow of blood.
In addition to causing unpredictable pain episodes, blood vessel blockage greatly increases the risk of heart attack, stroke, chronic kidney disease and pulmonary embolism, among other complications. “It’s a chronic disease requiring medications and control for life,” Costa said.
Hydroxycarbamide is the medication currently used to prevent this type of blockage (vaso-occlusion). The drug boosts the production of a protein called fetal hemoglobin, which hinders the polymerization of defective hemoglobin and mitigates the risk of vaso-occlusion.
In recent years, researchers at UNICAMP’s Blood Center have discovered other uses for the drug, such as preventing some of the complications that result from hemolysis, the rupture of red blood cells and the release of hemoglobin into the blood stream, which potentially leads to chronic inflammation (read more at: http://agencia.fapesp.br/22007).
The only treatment capable of curing sickle cell anemia, however, is a bone marrow transplant. In Brazil, the procedure has been covered by the SUS only since 2015. Many bone marrow transplants in patients with sickle cell anemia in Brazil, always involving compatible siblings, have been performed by the Center for Cell-Based Therapy (CTC), hosted by the University of São Paulo’s Ribeirão Preto Medical School (FMRP-USP). The CTC is a Research, Innovation and Dissemination Center (RIDC) funded by FAPESP.
The article notes that gene therapy has been considered promising as a treatment for SCD since the mid-1990s, but clinical trials have only recently begun, seeking FDA approval for a procedure using lentiviral vectors, which involves inserting genes engineered to reduce sickling into hematopoietic stem cells. The initial results have been promising.
Other approaches, such as CRISPR/Cas9 gene editing, which can replace a specific DNA region, are also considered promising for the treatment of SCD. This technique is currently used only in mice and cultured human cells.
Many ethical issues must be resolved before such techniques can be used in humans, the authors write: “Long-term follow-up trials will be needed to confirm their safety and sustainability, and the accessibility of gene therapy in high-burden, low-income areas needs to be addressed”.
As noted by the article, the burden of SCD is heavier on poor countries. In high- and middle-income countries, the clinical course of SCD has substantially changed since the 1970s in both children and adults. The survival of children with sickle cell anemia is similar to that of healthy children in the United States and the United Kingdom. In Africa, however, mortality rates range from 50% to 90% for children under 5 years of age with the disease. Adults with SCD in high-income countries can now expect to live well into their sixties.
Inequality of SCD distribution and care
The Brazilian Health Ministry estimates that between 30,000 and 50,000 people have some form of SCD in the country. Worldwide, 300,000-400,000 babies are estimated to be born with one of the genetic mutations each year, with 230,000 in sub-Saharan Africa alone.
Thanks partly to the PNTN national newborn screening program, Brazil has reliable epidemiological data and can take action before the symptoms of SCD appear. The heel prick test was officially implemented by the federal government in 2001, although it had already been in use for some time in certain parts of the country.
In fact, coverage is still highly unequal. In 2016, all hospitals in the state of Minas Gerais performed the heel prick test, while only approximately half did so in the state of Amapá, according to Costa.
Screening has enabled the authorities to estimate survival rates and the main causes of death among people with SCD. It is also the basis for the provision of prophylaxis, especially vaccination and the administration of penicillin before age 5 to avoid infections, which are the main cause of death.
Ensuring universal coverage is key because the distribution of SCD is so uneven. Sickle cell anemia is more common in the North and Northeast than in other regions of Brazil because the mutation that causes the disease is more prevalent among people of African ancestry, of whom there are many in those regions.
On the other hand, thalassemia, especially the most severe form, is more common among people of Mediterranean ancestry, such as the many descendants of Italian immigrants in the South and Southeast regions.
The article shows that in areas without screening programs for newborns, the initial diagnosis of SCD occurs at approximately 21 months of age. For many individuals, the first sign of sickle cell anemia is a fatal infection or an acute splenic sequestration crisis, when sickled red blood cells become trapped in the spleen in large numbers, causing a sudden enlargement of the organ that can be life-threatening. Early diagnosis and penicillin prophylaxis reduces mortality in the first five years from 25% to less than 3%, according to the article.
The problem is that accurate estimates of the number of sickle cell anemia patients are difficult to obtain, even with good healthcare systems and in countries with universal screening programs such as Brazil.
“Fortunately, the collection of epidemiological data is steadily improving. Geospatial and other sophisticated methods could produce fairly reliable estimates of the number of people with sickle cell anemia worldwide,” Frédéric B. Piel, a researcher at Imperial College London and one of the authors of the article, told Agência FAPESP.
“These projects depend on large collaborative networks for data collection and processing, and the ability to analyze big data, all of which requires substantial amounts of funding.”
The article “Sickle cell disease” (doi:10.1038/nrdp.2018.10) by Gregory J. Kato, Frédéric B. Piel, Clarice D. Reid, Marilyn H. Gaston, Kwaku Ohene-Frempong, Lakshmanan Krishnamurti, Wally R. Smith, Julie A. Panepinto, David J. Weatherall, Fernando F. Costa and Elliott P. Vichinsky can be read at: www.nature.com/articles/nrdp201810.
Source: https://agencia.fapesp.br/30729