

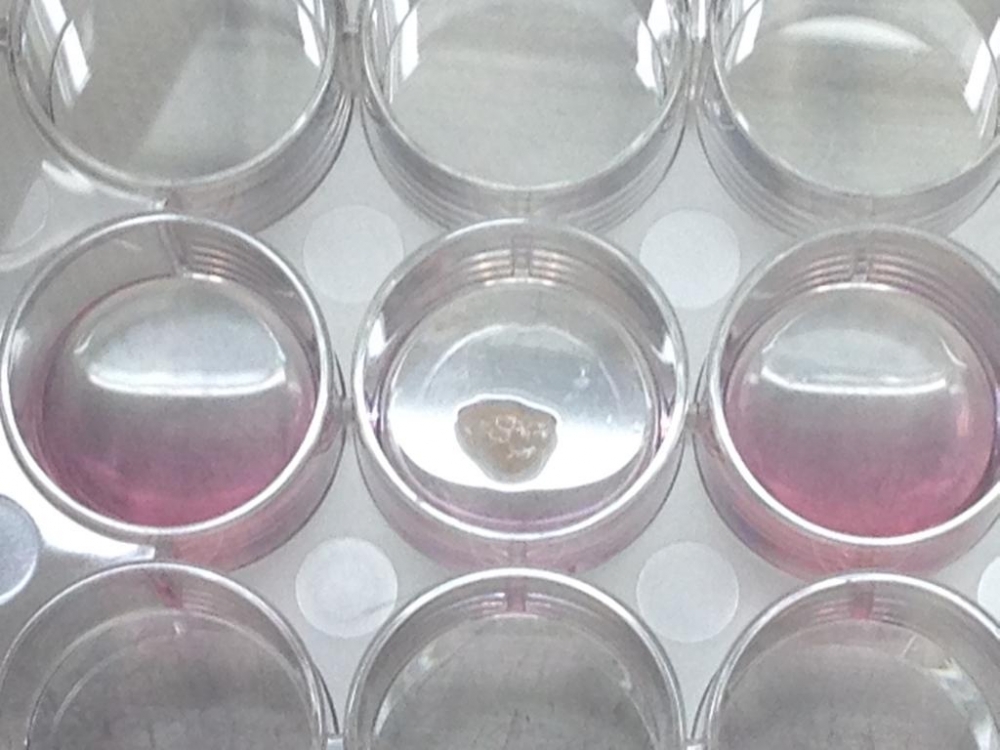
Brazilian scientists conducted preclinical trials to test membranes produced from mesenchymal stem cells that can differentiate to cartilage and promote local immunoregulation (extracellular matrix membrane produced by stem cells; photo: researchers’ archive)
Published on 05/10/2021
By Janaína Simões | Agência FAPESP – The surgical interventions available from the Brazilian health system to treat knee injuries are invasive and complex. Moreover, they do not always solve the problem. The alternative is using stem cells to produce membranes for implantation in the knee joint. In Brazil, research with this objective has been conducted by a group led by Tiago Lazzaretti Fernandes, an orthopedic surgeon affiliated with the Sports Medicine Center at Hospital das Clínicas, the hospital complex run by the University of São Paulo’s Medical School (FM-USP).
The scientists have already obtained positive results in preclinical trials (with animals) using membranes produced from mesenchymal stem cells in bone marrow, the knee fat pad and synovia, and dental pulp. These stem cells can differentiate into fat, bone and cartilage. “In over 15 years of research, there have been very few descriptions of tumor formation, although this is mentioned in studies on certain types of stem cell as a severe adverse side-effect. They’re very safe and widely used,” said Fernandes, co-author of a review article on the subject published in Frontiers in Immunology.
In the study, the researchers analyzed the efficacy of membranes produced from two sources of mesenchymal stem cells. One was the synovial membrane, a thin layer of tissue lining the most internal part of the joint. This tissue produces synovial fluid, which lubricates the joint to prevent damage. The other source of the stem cells used was dental pulp, thanks to a partnership with Daniela Franco Bueno at the Syrian-Lebanese Institute of Education and Research (IEP) in São Paulo. She studies the use of this method to treat cleft lip and palate.
According to Fernandes, there are several advantages to using mesenchymal stem cells. “Embryonic stem cells involve a number of ethical and religious conflicts that hinder research,” he said. “We could use induced pluripotent stem cells, which are similar to embryonic stem cells but produced from adult cells, but research suggests the risk of tumors is significant and we need more studies to clarify this point.”
Another advantage is that mesenchymal stem cells differentiate to cartilage cells, the goal of the research project supported by FAPESP. Besides Bueno, Fernandes’ group also includes Arnaldo Jose Hernandez, a professor at FM-USP.
More effective alternatives
Three surgical techniques are used to treat damage or injury to the cartilage that protects the inside of the knee joint. This tissue is about 3-4 mm thick and reduces friction in the joint as well as acting as a shock absorber. “When the knee cartilage is injured, we usually recommend physical therapy to strengthen the muscles, relieve pain and restore functionality. If there’s no improvement, surgery may be required,” Fernandes said.
None of the surgical techniques in current use is completely effective, he added. In one, the surgeon makes small holes in the region of the injury to bring about local bleeding. Blood accumulates in the region, forming fibrocartilage. “It’s a repair. The result isn’t new cartilage but a scar that enables the knee to function satisfactorily for two or three years, after which the pain and other symptoms return,” he said. A second option is to remove a small piece of bone and cartilage from a non-loadbearing part of the knee and graft it on to the injured part.
When the defect to be repaired is larger than the piece of cartilage that could be grafted, the surgeon uses a more complex technique involving a tissue transplant. “We remove the material from brain-dead donors, as is done with other organs,” he said.
Cell-based therapy
An alternative is autologous chondrocyte implantation (ACI), a cell-based therapy that uses the patient’s own cartilage cells. Available in Europe and the United States but not in Brazil, ACI starts with the arthroscopic harvesting of healthy cartilage from a non-loadbearing part of the knee. The cells are isolated in a laboratory, multiplied, and seeded in a collagen membrane. After 30 days the membrane with the cells is taken to the operating room and glued to the area of the lesion.
The group led by Fernandes deploys a similar technique to ACI using mesenchymal stem cells from the synovial membrane or dental pulp to produce an extracellular matrix or membrane.
In a study reported in Tissue Engineering and conducted at the Syrian-Lebanese Hospital in São Paulo, which has all the certifications required by scientific and medical regulations to process tissue for use in humans, the researchers collected, isolated and grew synovial membrane mesenchymal stem cells. Among the advantages of the technique is the fact that it can be used to treat larger lesions and does not require recourse to a tissue bank or donors because the cells are extracted from the patient. The purpose is not to regenerate tissue identical to that existing before the injury. “We aim to repair the knee so that its functionality is restored and the patient can move about normally without pain,” Fernandes said.
Another aim of the study was to evaluate the use of mesenchymal stem cells extracted from dental pulp. Membrane production in this case is the same as when synovial cells are used. When a child’s milk tooth is close to shedding, it is extracted by a dentist, sent to the laboratory and stored in liquid nitrogen as a source of cells. The difference resides in the quantity of cells extracted from the pulp and cell growth in the laboratory to generate the extracellular matrix that will be implanted in the knee. The researchers conducted a large-scale review of the literature to understand the possible uses of dental pulp cells to treat cartilage damage. This is also published in Tissue Engineering.
Preclinical trials
After these studies, the researchers conducted trials in large animals to see if dental pulp stem cell implantation could repair a lesion. They used miniature pigs, as reported in Stem Cell Reviews and Reports. “This animal has knees that closely resemble ours both anatomically and physiologically,” Fernandes said.
A six-millimeter lesion was created in the hind limbs, and one was treated with the tissue implant. “We performed paired statistical comparisons – whatever occurred on the right-hand side also happened on the left-hand side. Both knees were exposed to the same weight-bearing conditions, with no restrictions on load or movement,” he explained.
The analysis began six months after the engineered tissue was implanted. This was considered a sufficient amount of time for the cartilage to recover. Scientific articles on the trials are in press, but the results show that use of the membrane assured better recovery from the lesion in both treatments and that synovial cells are preferable to dental pulp cells. Once the articles have been published, the next step will be to conduct trials in human patients who already have lesions. Application has been made for the necessary permits for clinical trials in humans.
The Frontiers in Immunology article “Macrophage: A potential target for cartilage regeneration” by Tiago Lazzaretti Fernandes, Andreas H. Gomoll, Christian Lattermann, Arnaldo Jose Hernandez, Daniela Franco Bueno and Mariane Tami Amano is at: www.frontiersin.org/articles/10.3389/fimmu.2020.00111/full.
Source: https://agencia.fapesp.br/35826