

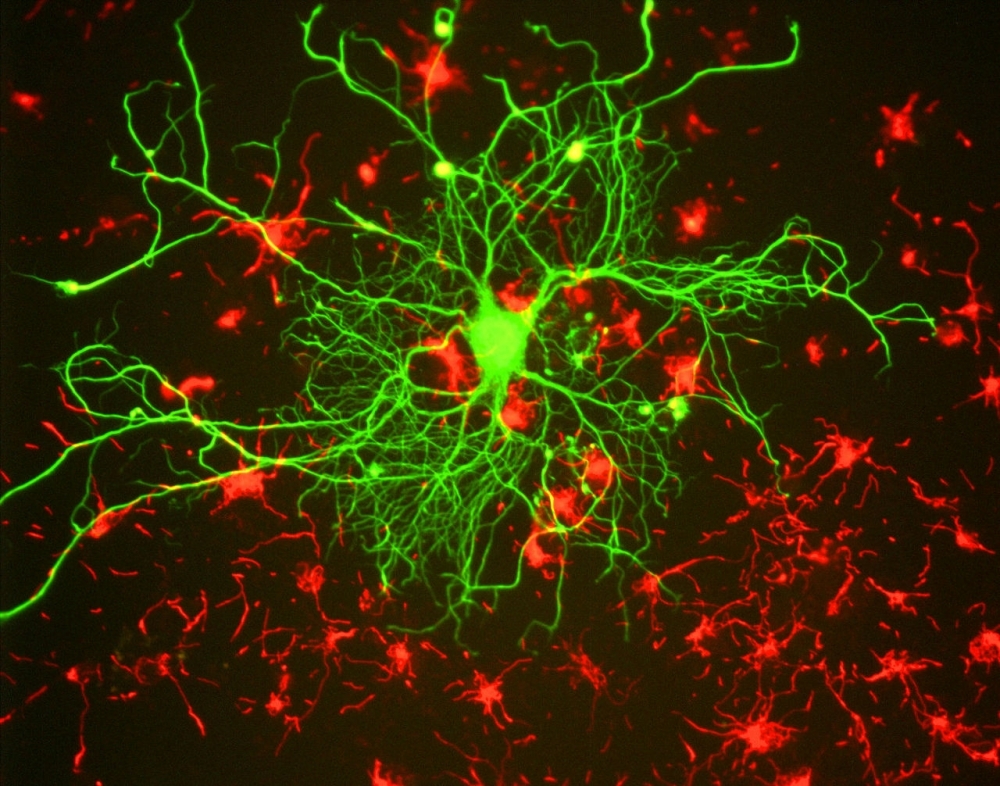
A group at the University of Campinas used protein mapping to show how abnormal levels of the neurotransmitter glutamate impair the functioning of neurons and oligodendrocytes. The findings could serve as a basis for more effective treatment (image: Gerry Shaw/Wikimedia Commons)
Published on 06/07/2021
By Luciana Constantino | Agência FAPESP – A study conducted by a group of Brazilian researchers contributes to a deeper understanding of the molecular basis for schizophrenia, and potentially to the development of more specific and effective treatments for the disease. The medications currently available on the market act generically on the brain and can have severe adverse side effects.
Treatment of post-mortem samples from the hippocampus of schizophrenic patients with an NMDA receptor antagonist pointed to biological processes associated with the disease that are specific to neurons and oligodendrocytes. NMDA receptors are neurotransmitter receptors located in the postsynaptic membrane of neurons, and receive signals across the synapse from previous nerve cells.
The antagonist in question was MK-801, a drug that alters the neurotransmitter function of glutamate, mimicking in vitro what happens in schizophrenia (glutamate is the brain's primary excitatory neurotransmitter). Neurons treated with the substance displayed oxidative stress, one of the factors that can lead to brain degeneration, and apoptosis (programmed cell death). Oligodendrocytes, which synthesize the myelin sheath that insulates axons, were not altered in the same way. On the other hand, oligodendrocytes displayed differences associated with protein synthesis and myelin membrane organization.
The Laboratory of Neuroproteomics at the Institute of Biology of the University of Campinas (UNICAMP) used post-mortem brain tissue samples from patients with schizophrenia. The results, obtained in collaboration with the group led by Helder Nakaya, a professor at the University of São Paulo’s School of Pharmaceutical Sciences (FCF-USP), are reported in an article published in European Archives of Psychiatry and Clinical Neuroscience.
“After culturing neurons and oligodendrocytes in the lab and treating them with MK-801, we analyzed the proteins in the brain and each cell type, cross-referencing the data. This enabled us to identify differences specific to neurons or oligodendrocytes, or common to both,” said Daniel Martins-de-Souza, principal investigator for the study and head of the laboratory, which is supported by FAPESP.
Previous research found abnormal levels of glutamate in the brains of schizophrenic patients and linked glutamatergic neurotransmission dysfunction to NMDA receptor hypofunction. Glutamatergic neurotransmission is essential for cognition, learning and memory in humans.
“The treatment of neural cells with MK-801 revealed that neurons, oligodendrocytes and astrocytes are affected but present different responses to NMDA receptor hypofunction. NMDA receptor activation in oligodendrocytes is involved with their maturation, metabolic modulation and myelination around axons,” the researchers write in the article.
An axon is part of a neuron that carries nerve impulses away from the cell body. Each neuron typically has one axon that connects it with other neurons via their synapses. Its filaments are insulated by a sheath made of myelin, a lipid-rich substance that prevents loss of energy during the transmission of electrical impulses between neurons.
“Thus, understanding the effects of glutamatergic dysregulation in both neurons and oligodendrocytes is crucial to a grasp of the role of these cellular counterparts in schizophrenia, especially in the hippocampal context,” the article continues, adding that “we were able to find proteomic signatures in common between the hippocampus and MK-801-treated neurons, and between the hippocampus and the MK-801-treated oligodendrocytes”. These findings will contribute to the development of treatments better targeted to the different dysfunctional biological processes in the various brain cell types.
According to PhD candidate Giuliana da Silva Zuccoli, first author of the article, lack of myelin or improper sheath formation may be part of the reason for cognitive and memory problems in schizophrenia.
Last year a study conducted at UNICAMP’s Laboratory of Neuroproteomics with FAPESP’s support had associated schizophrenia with dysfunctional oligodendrocytes that produce defective myelin.
FAPESP also supported the research that resulted in the article through funding for six other projects: 2018/14666-4, 2017/25588-1, 2019/00098-7, 2017/50137-3, 2012/19278-6 and 2013/08216-2.
23 million cases worldwide
Considered a severe debilitating mental disorder, schizophrenia affects some 23 million people worldwide, including 1.5 million Brazilians, according to the Pan American Health Organization (PAHO). It is characterized by thoughts or experiences that seem out of touch with reality, disorganized speech or behavior, and reduced participation in daily activities. Treatment involves a combination of medications, psychotherapy and specialized care. A clinical assessment is required to diagnose schizophrenia.
A promising methodology was developed last year to create a blood test that can diagnose schizophrenia by Brazilian researchers affiliated with the Federal University of São Paulo (UNIFESP) and UNICAMP. The test is the first to detect the disorder by analyzing biochemical and molecular alterations (more at: agencia.fapesp.br/34356).
The article “Linking proteomic alterations in schizophrenia hippocampus to NMDAr hypofunction in human neurons and oligodendrocytes” by Giuliana S. Zuccoli, Guilherme Reis-de-Oliveira, Bruna Garbes, Peter Falkai, Andrea Schmitt, Helder I. Nakaya and Daniel Martins-de-Souza can be retrieved from: link.springer.com/article/10.1007/s00406-021-01248-w.
Source: https://agencia.fapesp.br/36053