

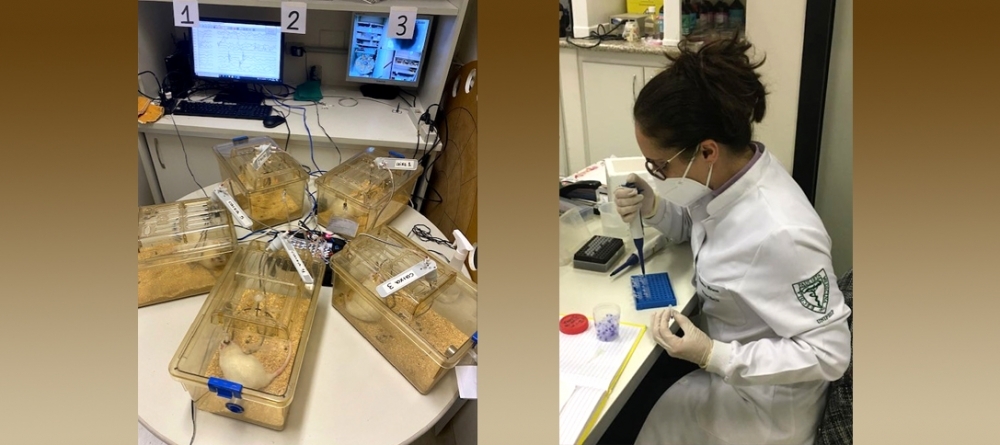
Photos: researchers’ archive
Published on 08/21/2023
By Cristiane Paião | Agência FAPESP – In Brazil, researchers at the Federal University of São Paulo’s Medical School (EPM-UNIFESP) have conducted experiments with animals to find out whether frequent deep brain stimulation (DBS) can help control epilepsy, a neurological disease in which nerve cell activity in the brain is disturbed by abnormal electrical discharges, causing seizures.
The results of the study are reported in an article published in the journal Brain Stimulation.
Led by Professor Luciene Covolan, the study showed that stimulation of the anterior nucleus of the thalamus by means of electrodes implanted in the central part of the brain achieved long-term suppression of epileptic seizures in rats by increasing the production of adenosine, a substance resulting from cell energy metabolism with an important role in communication among neurons.
The study was part of the project “The roles of adenosine to prevent epileptogenesis through anterior nucleus of thalamus deep brain stimulation”, conducted with support from FAPESP. The research is continuing and is now in a new stage, in partnership with Rutgers University in the United States.
“When a person has epilepsy, they have too much adenosine kinase [ADK] in the brain. This enzyme is responsible for neuron DNA methylation, a biochemical modification that alters gene expression. Basically, it alters the functioning of cells and may be one of the factors that lead to epileptic seizures. When we observed that the increase in adenosine due to deep brain stimulation lowered ADK levels, we also noted a reduction in seizures and concluded that a sort of reprogramming of the neurons involved in seizures may occur. Our hypothesis is that when the anterior nucleus of the thalamus is stimulated, the increase in adenosine and decrease in ADK lead to attenuation of the seizures, and even remission in some cases, via transmethylation of the DNA present in the cells of these brain circuits,” Covolan told Agência FAPESP.
The hypothesis being tested in the rat experimental model is modification of brain tissue DNA. “Deep brain stimulation reduces seizures gradually during the treatment. They don’t just suddenly stop. This suggests the role of adenosine may not be confined to acting on its receptors but may also be involved in several other mechanisms. One of these, for example, could be stabilization of neuron membrane electric potential. This is a mechanism we mean to investigate more thoroughly, but there’s ample evidence that it could be the case,” Covolan said.
The discovery is important, she added, because in future it may contribute to the development of less invasive treatment for patients not indicated for surgery. “Our view of this adenosine mechanism is that we’re ‘teaching’ cells to return to normal. If we’re right, we could start thinking about strategies and treatments for epilepsy as such, rather than just reducing the frequency of seizures, as we’ve done so far,” she said.
More than 50 million people have epilepsy worldwide, including some 3 million Brazilians, according to the World Health Organization (WHO). About 70% of cases are controlled with medication, but there are few alternatives for the 30% who do not respond to drugs. They include surgical resection to remove the seizure focus from the brain. When this area is well-defined in the patient, the probability of long-term control is reasonably high, but it is not always possible to detect where seizures start. Even when this can be done, resection may not be successful.
The main motivation for the UNIFESP group’s experiments with rats is to look for other approaches to treatment, especially for temporal lobe epilepsy, which accounts for 30% of cases.
The surgical procedure to implant electrodes for deep brain stimulation has recently been approved in the US and Brazil. It is considered an alternative for patients who do not respond to medication. Clinical trials have shown that seizure frequency improves in a high proportion of such cases, but the action mechanism is poorly understood.
“In 2010, another group of researchers announced the important clinical finding that epileptic patients who underwent surgery to have electrodes implanted in the anterior nucleus of the thalamus benefited from a gradual reduction in seizures over years of stimulation. Many even stopped having any seizures at all after two to five years of treatment, with a significant improvement in quality of life, but it remained to find out now and why this happened,” Covolan said.
The role of the thalamus in epilepsy
The thalamus is sometimes considered an “on/off switch” for consciousness. Located in the center of the brain between the cerebral cortex and the midbrain, it receives signals from sensory pathways and distributes them to the cortex. It also makes important connections between the systems involved in limbic epileptic seizures. Whenever a seizure starts in a region of the cortex, the information necessarily passes through the thalamus and from there to the rest of the circuit, returning to the cortex and manifesting in the patient. This is why the UNIFESP group chose the thalamus for their study, Covolan explained. “When we investigate what happens in deep brain stimulation, our overall aim is to prevent information from a seizure happening in a particular point of the brain from spreading to other areas,” she said.
The clinical manifestation of a seizure relates to the brain region in which it begins. It can be over quickly or last quite a long time. It may or may not involve alterations of consciousness, with motor or sensory phenomena. It may be single or multiple. And it may occur while the patient is awake or asleep. All this depends on where it originates in the brain.
“It’s like an orchestra. The nervous system prepares to give a response, and the thalamus is the conductor. The circuit includes the hippocampus and other limbic structures that characterize temporal lobe epilepsy,” Covolan said. “Transmission of information by the thalamus to the cortex can be inhibited by deep brain stimulation. Epileptic seizures trigger muscle contraction and can lead to loss of consciousness, but motor systems are only affected if the seizure reaches the motor cortex, which gives the spinal cord orders for muscles to contract. Can a seizure in the hippocampus fail to reach the cortex? Yes, and this is exactly what we’re trying to do by modulating neuronal activity so that seizures don’t reach the cortex intensely enough to trigger discharges in the patient or lead to loss of consciousness.”
Next steps
The researchers now want to understand how neuron DNA methylation happens and cell functions change after ADK is reduced, among other things. According to Covolan, this will involve measuring the methylation precisely in further experiments. They also need to find out which novel substances or drugs could be developed to help patients, based on this knowledge of the action mechanism involved in deep brain stimulation to treat epilepsy.
“We’re conducting a systematic review of the experimental models of epilepsy that use deep brain stimulation and analyzing large amounts of data. We plan to perform more complex analyses of DNA in order to find out what’s actually changing, whether this methylation or transmethylation produces different proteins that are then transcribed, whether the DNA changes after stimulation. These experiments will be costly. We plan to submit other projects, and it would be great if we have a product, perhaps a patent,” Covolan said.
The other participants in the research were Christiane Gimenes, Maria Luiza Motta Pollo and Eduardo Díaz at UNIFESP’s Department of Physiology; Eric Hargreaves at Jersey Shore University Medical Center; and Detlev Boison at Rutgers University’s Robert Wood Johnson Medical School. Díaz is currently a PhD candidate at the Albert Einstein Jewish Institute of Education and Research (IIEP-SBIBAE) in São Paulo.
The article “Deep brain stimulation of the anterior thalamus attenuates PTZ kindling with concomitant reduction of adenosine kinase expression in rats” is at: www.brainstimjrnl.com/article/S1935-861X(22)00099-7/fulltext.
Source: https://agencia.fapesp.br/42192