

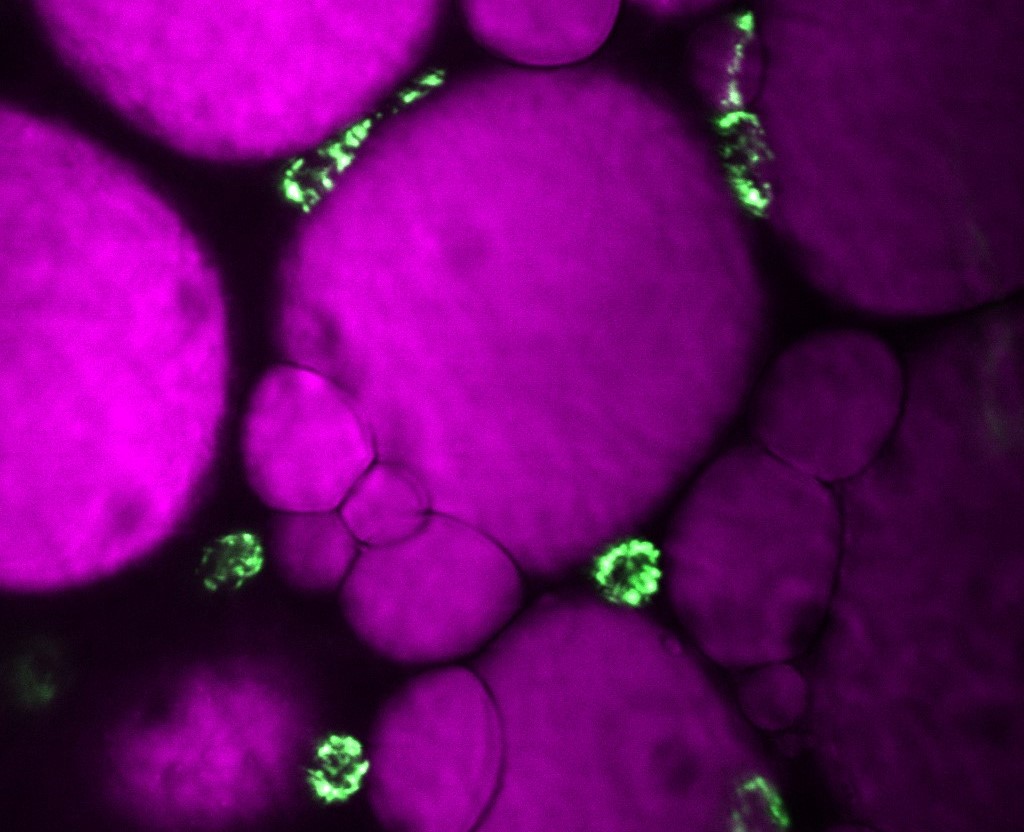
Visceral adipose tissue cells (purple) and adipose tissue-resident innate immune cells (green) (credit: Monara Angelim)
Published on 07/02/2024
By Karina Toledo, from Shenzhen | Agência FAPESP – Already at the beginning of the COVID-19 pandemic, a group of Brazilian researchers pioneered in showing why SARS-CoV-2 infection tends to be more severe in diabetic patients. Now, the same team based at the Institute of Biology of the State University of Campinas (IB-UNICAMP) has discovered one of the reasons why obese people who do not have diabetes or even insulin resistance also have an increased risk of developing the severe form of the disease.
“New experiments show that the molecular mechanisms are quite different in the two cases,” Pedro Moraes-Vieira, a professor at IB-UNICAMP, who is coordinating the research, told Agência FAPESP.
The research is supported by two projects (20/16030-0 and 20/04579-7) and is also linked to the Obesity and Comorbidities Research Center (OCRC) – a FAPESP Research, Innovation and Dissemination Center (RIDC) based at UNICAMP.
The data were presented on June 29 at a panel discussion on health and biomedicine as part of the FAPESP Week China program. Also present at the panel were Zhang Zhiyong, from Guangzhou Medical University, Luciana Cezar de Cerqueira Leite,from Butantan Institute; Xin Jin, chief research scientist at the Chinese company BGI, and Dan Zhang, cofounder of Chinese company Hillgene BioPharma. Xin Jin and Simone Appenzeller, from UNICAMP, acted as the panel’s mediators.
In an article published in May 2020, the UNICAMP group showed that in diabetics infected with SARS-CoV-2, the higher glucose content in the blood is picked up by a type of defense cell known as monocytes and serves as an extra source of energy that allows the virus to replicate more than in a healthy organism. In response to the growing viral load, the monocytes release large amounts of cytokines (inflammatory proteins), which cause a variety of effects, including the death of lung cells. The researchers also reported that in the lungs of patients with severe COVID-19, monocytes and macrophages were the most abundant cells. And that the so-called glycolytic pathway, which metabolizes glucose, was greatly increased in these leukocytes (read more at: agencia.fapesp.br/33296).
The latest study, the results of which should be published soon, shows that hyperinflammation in obese non-diabetics is linked to elevated blood levels of saturated fatty acids – particularly a type known as palmitate. Also known as palmitic acid, it is the main component of palm oil. It is found in beef, milk and its derivatives.
“Through in vitro experiments, we observed that palmitate promotes a pre-activation of innate immunity cells [the first to take action in the face of an infection]. They become alert, ready to respond more intensely if they detect a threat. When we infect these pre-activated cells with SARS-CoV-2, they produce a greatly increased amount of inflammatory cytokines,” explains Moraes-Vieira.

IB-UNICAMP professor Pedro Moraes-Vieira (photo: Karina Toledo/Agência FAPESP)
Impaired immunity
In previous work, the UNICAMP group had already observed that, in the context of COVID-19, this “cytokine storm” produced by monocytes and macrophages is the basis of two very undesirable phenomena: the death of lung epithelial cells and the dysfunction of the adaptive immune response – the one that kicks in about two weeks after infection and is related to the action of cells (mainly T lymphocytes) capable of recognizing and killing pathogens in a specific way.
“When we cultured the T cells in a medium conditioned by monocytes infected with SARS-CoV-2, we saw a lower proliferative capacity, reduced secretion of inflammatory cytokines, and increased expression of a protein called PD-1, whose role is to signal to the T lymphocytes when it is time to stop responding to the infection. The idea is that this signaling occurs after a while so that there is no exacerbated immune response. In the context of severe COVID-19, however, PD-1 causes T lymphocytes to stop working even before the disease is resolved, leading to a process called exhaustion, which is common in T cells found in tumors, for example, and is associated with a worse prognosis,” the researcher explains.
“These findings help us understand why non-diabetic obese people are also more likely to develop severe COVID. Of course, this is not the only factor. But we are adding another piece to the puzzle,” concludes Moraes-Vieira.
To find out more about FAPESP Week China, visit: fapesp.br/week/2024/china.
Source: https://agencia.fapesp.br/52126