

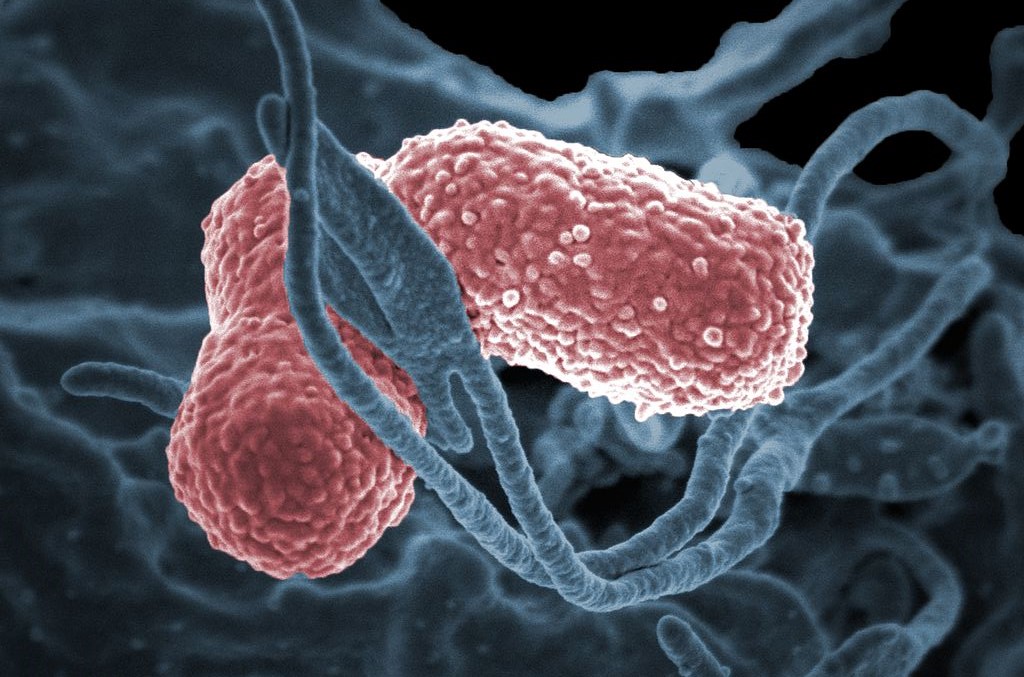
The bacteria detected most frequently in the study was Klebsiella pneumonia, which can cause pneumonia and bloodstream infections (image: NIAD/Wikimedia Commons)
Published on 10/02/2023
By Luciana Constantino | Agência FAPESP – Rapid identification of patients contaminated by “superbacteria” known as “carbapenem-resistant Enterobacteriaceae” (CRE), with early isolation of these patients, reduces transmission in hospital emergency departments. However, keeping them in the emergency room (ER) for more than two days undermines containment because it increases the risk of infection via colonization.
These are the key findings of a study by a group at the University of São Paulo’s Medical School (FM-USP) in Brazil. An article on the study is published in the journal Clinical Infectious Diseases.
Enterobacteria are gram-negative bacteria that cause infections in hospitals and clinics. They include Escherichia coli, a cause of urinary infections and hemorrhagic colitis, and Klebsiella pneumoniae, which can lead to pneumonia and bloodstream infections. CRE are considered a threat to public health because they are hard to treat. Carbapenem antibiotics are usually the last line of defense against infections caused by these microorganisms.
“Our study focused on an intervention in an overcrowded ER, a hotspot for CRE transmission. We found that the intervention reduced CRE transmission in the ER and the rest of the hospital,” Matias Chiarastelli Salomão, first author of the article, told Agência FAPESP. He is an infectious disease specialist and a member of the Hospital Infection Control Subcommittee at the Central Institute of Hospital das Clínicas (HC), the hospital complex run by FM-USP.
Previous research conducted in the ER showed that 6.8% of admitted patients were colonized by CRE and 18% were contaminated during their stay in the ER.
According to a report published in 2022 by the World Health Organization (WHO), seven out of every 100 patients admitted to acute-care hospitals are infected with at least one healthcare-associated infection (HAI) during their hospital stay in high-income countries, and 15 in low- and middle-income countries. One in ten die as a result on average.
The aims of the study, Salomão explained, included trying to understand and seek alternative ways of preventing infections acquired in the ER from spreading to other parts of the hospital. “The intervention was pragmatic and can be applied elsewhere. As for the finding that an ER stay of more than two days impairs containment, we see this as due to the fact that the ER’s structure wasn’t equipped for long-stay patients. In other words, beds were too close together and hand hygiene stations too far apart, among other problems,” he said.
Methodology
The study was conducted in the ER of Hospital das Clínicas, which has 800 beds but is often so overcrowded that it holds double that number, some of whom stay for more than 11 days.
FAPESP supported the study via a regular research grant awarded to Icaro Boszczowski, last author of the article.
The study was divided into two phases, a baseline phase on February 3-28, 2020, before the first COVID-19 patient was admitted to the hospital, and the intervention proper, from September 14 to October 1, 2022. The hospital was entirely dedicated to COVID-19 cases from April 1 to August 31, 2020, after which it was gradually reopened for other types of patient.
Phase 1 focused on determining the prevalence and incidence of patients colonized by CRE admitted to the ER. Patients who stayed in the ER for longer than 24 hours occupied beds and gurneys in close proximity to each other while waiting to be transferred.
In phase 2, the intervention, patients admitted to the ER were screened for CRE during the first 24 hours of their stay. If they tested positive for superbacteria, they were isolated until discharge – 90% of those isolated were infected by Klebsiella pneumoniae. Cleaning and disinfection procedures were similar and antimicrobial use was monitored in both phases.
The results obtained by culture and molecular test showed that colonization at admission was 3.4% and that CRE infection acquisition rates fell from 4.6% to 1% during the intervention. A stay of more than two days in the ER was a significant risk factor for CRE acquisition.
“The idea for the study began at the hospital, as all intensive-care patients had been routinely screened for CRE on admission to the ICU and every week thereafter since 2014, and secondary colonization rates had fallen significantly as a result. However, another study found that superbacteria were entering via the ER,” said Salomão, who first studied the problem for his PhD research.
Two other articles resulted from the work done in this period, the latest of which was published in Emerging Infectious Disease in 2020.
The article “Transmission of carbapenem-resistant Enterobacterales in an overcrowded emergency department: controlling the spread to the hospital” is at: academic.oup.com/cid/article/77/Supplement_1/S46/7219531?login=false.
Source: https://agencia.fapesp.br/49872