

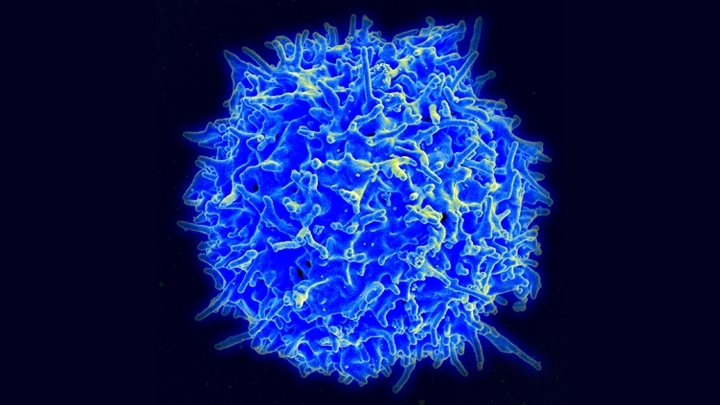
Brazilian researchers found the novel coronavirus replicating inside immune cells from patients hospitalized with COVID-19. Experiments on lymphocytes infected in the laboratory showed that viral entry induced programmed cell death (B lymphocyte. Image: NIAD/NIH)
Published on 03/18/2021
By Karina Toledo | Agência FAPESP – Experiments conducted at the University of São Paulo’s Ribeirão Preto Medical School (FMRP-USP) in Brazil have shown that the novel coronavirus can infect and kill various types of lymphocyte, key cells in the organism’s defense against pathogens. The researchers do not yet know for sure whether immunity is weakened as a result, or for how long, but they believe infection of lymphocytes may cause long-term damage to the immune system.
The study was supported by FAPESP. A paper reporting the results is published on the preprint platform bioRxiv. The paper is currently being peer-reviewed.
“In the early days of the pandemic, scientists noticed that lymphopenia [abnormally low levels of lymphocytes in the blood] was a frequent hematological alteration in hospitalized COVID-19 patients and was associated with a poor prognosis, a higher risk of intubation and death. However, the cause of the problem wasn’t properly understood until now,” Eurico Arruda, Professor of Virology at FMRP-USP and principal investigator for the study, told Agência FAPESP.
During a viral infection, he explained, it is expected that some defense cells will leave the bloodstream and migrate to the infected tissue to combat the invader. However, autopsies of patients who died from the severe acute respiratory syndrome associated with SARS-CoV-2 have shown that the quantity of lymphocytes present in infected tissues was not sufficient to account for the lymphopenia detected while the patients were still alive in the hospital.
“We realized some other mechanism must be involved and decided to find out whether defense cells in COVID-19 patients contained the virus,” Arruda Neto said. “Other research groups had reported that viral load was practically undetectable in blood, but they had analyzed whole blood. We isolated peripheral mononuclear blood cells [immune system cells such as lymphocytes and monocytes] and then made a sort of lymphocyte concentrate.”
Before they analyzed the patients’ immune cells, however, the researchers performed several experiments on blood samples from five healthy volunteers to test the hypothesis that SARS-CoV-2 was capable of infecting and killing lymphocytes.
The mononuclear cell concentrate obtained from the blood samples donated by healthy controls was incubated with the virus for two days. With an antibody capable of recognizing antigens of the virus in the cells, the researchers proved that infection had occurred. The analysis showed that monocytes were the mononuclear cells most susceptible to SARS-CoV-2 (44% were infected), followed by CD4+ T lymphocytes (which coordinate immune defense by releasing signaling molecules called cytokines: 14%), CD8+ T lymphocytes (which recognize and kill cells infected by the virus: 13%), and B lymphocytes (which produce antibodies: 7%).
Viral load in the cellular concentrate was measured after six, 12, 24, and 48 hours using RT-PCR, the molecular testing method to diagnose COVID-19, and was found to increase consistently, with a hundredfold growth in the last measurement. This result showed that the virus had entered the mononuclear cells and was replicating inside them.
“When we treated the culture with a compound that inhibits the protease used by SARS-CoV-2 to replicate, we observed a significant decrease in viral load,” Arruda Neto said. “This was one more proof that the virus was replicating in these cells, although as yet we don’t know exactly in which ones.”
In another experiment, the group tried to block infection with an inhibitor of ACE-2, the protein used by the virus to enter human cells. ACE-2 is normally expressed in small amounts in peripheral blood mononuclear cells.
“Treatment with the ACE-2 inhibitor reduced viral load in the culture but didn’t eliminate it completely, suggesting the existence of an alternative infection mechanism in lymphatic cells. This isn’t unusual in viruses, which can use different molecules to bind to different types of cells. Examples include HIV and adenoviruses,” Arruda Neto said.
Further investigation of infected CD4 and CD8 cells showed that viral penetration triggered apoptosis, or programmed cell death. According to Arruda Neto, this may explain the lymphopenia observed in COVID-19 patients.
Natural infection
The next stage of the investigation involved mononuclear cells from 22 patients treated in intensive care units (ICUs) for moderate to severe COVID-19. The material was collected between April 7 and June 18 at Hospital das Clínicas, the general and teaching hospital run by FMRP-USP.
The analysis showed that not all samples were infected, with proportions varying widely (from 0.16% to 33.9%). “The patients had different clinical profiles and were in different stages of the disease, making comparison difficult, but the fact is that we succeeded in confirming the presence of the virus inside mononuclear cells from COVID-19 patients,” Arruda Neto said.
The group selected samples from 15 donors to analyze the differences in proportions of cells infected by SARS-CoV-2, stratifying the patients by the time between the onset of symptoms and sample collection. The highest proportion of infected cells was found in B lymphocytes, possibly explaining why antibodies are not detected in some people after infection. This theory is currently being investigated.
In the case of monocytes, the more advanced the disease the higher the proportion of infected cells. The result for CD4 cells was similar.
Using immunofluorescence and confocal microscopy, the scientists confirmed the presence of double-stranded viral RNA inside the infected cells, showing that the virus was replicating, as its genome consists of a single strand of RNA.
“In aggregate, the data suggests that the virus can infect lymphocytes and replicate in them,” Arruda Neto said. “This is a potential complication, as it may make patients susceptible to opportunistic infections and hospitals are brimming with drug-resistant bacteria. Medics must watch out for this possibility. In addition, we don’t yet know what kind of delayed effect this may have on the immune system. The only way to find out is by means of follow-up research on convalescent patients.”
The research also received support from FAPESP via a postdoctoral scholarship awarded to Ronaldo B. Martins, a PhD scholarship awarded to Marjorie C. Pontelli, and a PhD scholarship awarded to Ítalo A. Castro. Martins, Pontelli and Castro are the first three authors of the article “Infection of human lymphomononuclear cells by SARS-CoV-2”, which can be read at: www.biorxiv.org/content/10.1101/2020.07.28.225912v2.full.pdf.
Source: https://agencia.fapesp.br/34407