

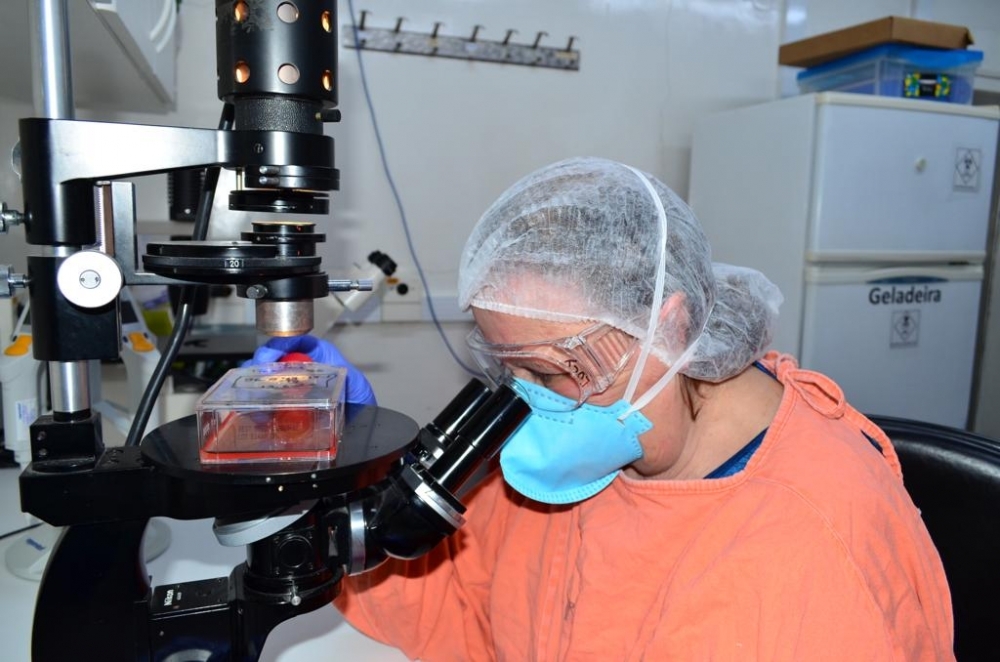
The material can be used for diagnostic testing, research on the evolution of the monkeypox virus, and development of novel treatments and vaccines (Professor Lucy dos Santos Vilas Boas working at LIM52; photo: Almir R. Ferreira (SCAPI/IMT/FM-USP))
Published on 06/27/2022
By Karina Toledo | Agência FAPESP – After completing the first genome sequencing of the monkeypox virus (MPXV) in Brazil, scientists at the University of São Paulo (USP) are culturing the virus in cell lines with the aim of distributing samples to public and private laboratories throughout the country for use in diagnostic testing, research on the evolution of the virus, and development of novel treatments and vaccines.
The work is ongoing at the Virology Laboratory (LIM52) of the Institute of Tropical Medicine (IMT-USP), and led by virologist Lucy dos Santos Vilas Boas.
“We received a clinical sample from the first patient diagnosed in Brazil and inoculated it into a culture of Vero cells. After 24 hours, we were able to observe morphological changes in the cells that are typical of monkeypox. This was confirmed by RT-PCR,” Vilas Boas told Agência FAPESP. Vero cells are derived from kidney epithelial cells extracted from an African green monkey, and widely used as a model for studying viruses.
The specific RT-PCR test for MPXV was developed at the Albert Einstein Jewish Hospital (HIAE) in São Paulo by a team led by Dr. João Renato Rebello Pinho, who is also a researcher at IMT-USP. The method is the same as for diagnosing COVID-19 and many other viral diseases, but each pathogen requires specific reagents so that the genetic material present in the clinical sample can be amplified and detected in the laboratory.
“Until that day [June 10], no lab anywhere in Brazil had a RT-PCR kit set up for this virus,” Pinho said. “We’d already studied the sequence [of nucleotides complementing the viral DNA, required to amplify the genetic material during the test] and asked a Brazilian firm to synthesize it. All that was missing was a positive control, which we obtained from the first confirmed local case. The positive control guarantees the test is working. Just like in the case of COVID-19, we’re seeing large-scale collaboration between public and private institutions, which is really important.”
After confirmation that the virus that multiplied in the Vero cells was a monkeypox virus, the next step was to extract it from the culture medium and inactivate it so that it could be shipped safely to other centers, Vilas Boas explained. “Infected cells die and release viral particles into the supernatant – the nutrient-rich liquid in which the cells are cultured. We collect this liquid and add a reagent that inactivates the virus,” she said. “We’re now sending samples of this material to public and private labs that have asked for them. At these other centers, the viral DNA can be extracted and used as a positive control in RT-PCR tests, expanding the nation’s testing capacity.”
According to José Eduardo Levi, a researcher affiliated both with IMT-USP and the DASA diagnostic laboratory chain, 96-well plates are typically used in RT-PCR tests, each with the capacity for clinical samples from 94 individuals, plus two for the positive and negative controls required to validate the results.
“The negative control can be water or supernatant from a virus-free cell culture. It’s hard to obtain a positive control when you’re dealing with a novel pathogen. Without it, you simply can’t be sure the RT-PCR test is actually working,” Levi said.
Despite the progress achieved, he added, specific reagents for MPXV are scarce in Brazil, and this is a major obstacle to mass testing for monkeypox if it should become necessary.
“When a US lab orders reagents, they arrive the next day because there are companies that specialize in producing reagents. In Brazil, they have to be imported, which takes at least a month. Here at DASA, we ordered them in early June but they haven’t arrived yet,” he said.
Large-scale production
Viral samples that can still infect cells and replicate are being delivered by IMT-USP to other high-level biosafety facilities. A case in point is the University of São Paulo’s Biomedical Sciences Institute (ICB-USP), which has a biosafety level 3 (BSL3) laboratory.
“Our job will be to cultivate the virus on a larger scale and start distributing aliquots to labs nationwide within two to three weeks. This will be made possible by an agreement we signed with the Science, Technology and Innovation Ministry [MCTI] and Post Office [ECT] at the start of the COVID-19 pandemic for specialized shipping of samples, which are picked up here and delivered directly to the addressee,” said Edison Luiz Durigon, Professor of Virology at ICB-USP and head of its BSL3 facility.
ICB-USP’s BSL3 laboratory is part of RedeVírus, a network set up by MCTI in February 2020 to provide input on science, technology and innovation strategies for the healthcare industry. The facility was responsible for large-scale production of SARS-CoV-2 and distribution of samples to diagnostic laboratories and research institutions nationwide.
The team has vast experience in this kind of work and has played a key role in successive public health crises. “It all began around 2003 with the Viral Genetic Diversity Network [VGDN], which was funded by FAPESP,” Durigon explained. “At that time, we cultured and distributed SARS-CoV-1 [the severe acute respiratory syndrome coronavirus that caused the 2002-04 SARS outbreak]. In 2005 we did similar work with the flu virus in 2005, and with zika virus in 2015. We received a sample from a zika patient from Evandro Chagas Institute in Belém [Pará state], and with resources from FAPESP-funded projects we cultured and distributed the virus to several labs. With the onset of the coronavirus pandemic and the agreement with MCTI, we were able to scale up the work we do.”
This has only been possible because the laboratory already had the necessary material and human resources, according to Durigon. “I had staff who had been trained thanks to master’s and doctoral scholarships awarded by FAPESP. If we’d had to start from scratch, it would have taken at least a year to get under way. You need proper infrastructure and continuous funding to respond quickly to a public health crisis such as a pandemic,” he said.
Besides large-scale production of MPXV, Durigon and his group will now sequence a number of samples to find out whether they differ from the monkeypox virus first isolated in Brazil. “In most cases, I expect we’ll distribute inactivated viral aliquots for use as positive controls by diagnostic centers. We’ll send viable viral samples for research only to the few labs that are BSL3 certified,” Durigon said.
For Ester Sabino, a professor at the University of São Paulo’s Medical School (FM-USP) and leader of Brazil’s first MPXV genome sequencing project, this is one more example of the significance of public universities in contributing to crisis responses because of their installed capacity. “Viral isolation is important not only for the production of positive controls but also for the evaluation of new drugs,” she said.
Pinho stressed the need for virologists nationwide to collaborate in networks, as well as the need for more investment in science.
Source: https://agencia.fapesp.br/38990